This podcast is available on Apple Podcasts, Stitcher, PlayerFM, iHeartRadio, Libsyn, Spotify, and Amazon Music.
Articles contain affiliate links. For more information on affiliate links, click here
Who You’ll Hear
Kati Kleber, MSN RN – Nurse educator, former cardiac med-surg/stepdown and neurocritical care nurse, author, speaker
Elizabeth Mills, BSN RN CCRN – highly experienced neurocritical care nurse, current Stroke Navigator for a Primary Stroke Center
What You’ll Learn
- Peripheral venous catheters / peripheral IV’s / PIV’s
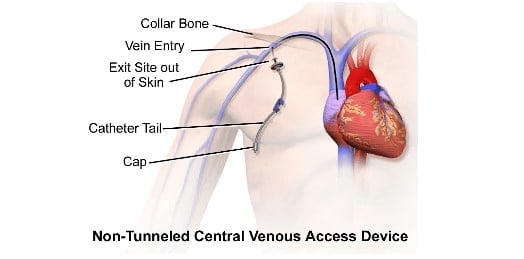
- Central venous catheters / CVC / central lines
- Care of CVC’s – everything is the nurse’s responsibility!
Peripheral venous catheters / peripheral IV’s / PIV’s
- Medscape: Intravenous Cannulation Overview
- It’s up to the nurse to decide the catheter size and insertion location
- The smaller the number, the larger the catheter
- Most adult patients will have an 18-20 gauge catheter
- The antecubital space (bend of the arm) is typically a great location for quick access, however if the patient has a continuous infusion, every time they bend their arm their IV pump will alarm
- The forearm is the ideal space, as there are no bends and it can be secured well
- Nurses are responsible for inserting peripheral venous catheters
- Make sure you look up your facility’s policy on insertion and frequency of removal
- Previous practice was to change IV site every 3 days, regardless of its condition, however, research is showing that this is not associated with better outcomes and therefore renders this action needless
- NCBI: Optimal timing for peripheral IV replacement?
- YouTube Example – Venipuncture Skill: Learning how to start an IV
Central venous catheters / CVC / central lines
- Wikipedia: Central venous catheter
- Please read the article before you hate on Wikipedia! This article has really great pictures and concise definitions
- Inserted by an advanced practice provider (PA, NP) or nurse with specialty training
- Inserted for various reasons: long-term antibiotics, vasoactive medications, TPN administration, monitoring central venous pressure (although there are newer, more accurate technologies available for this now), administration of large amounts of fluid, and so forth.
- You can draw blood from them, which is very helpful/convenient
- Various locations for insertion: subclavian, internal jugular, femoral
- Think of it as a really long IV, which starts outside of the skin and ends at or around the superior vena cava (SVC)
- If you’re not sure if it truly is a central line, then look at a chest x-ray and see where the tip terminates
- It is a line straight from the outside world to the patient’s heart, therefore infection is a MAJOR concern
- Central line blood stream infections (CLABSI’s) are the name for when a patient gets an infection because of their central line. People die from these.
- Strategies to Prevent Central Line-Associated Bloodstream Infections
- CDC resources for CLABSI’s
- Be Mr. Clean with central lines… this is a BIG DEAL for the nursing staff because while an infection can occur due to improper insertion, it’s more likely to occur because of improper care… and nurses are responsible for caring for, cleaning, and accessing them.
- Why are CVC’s needed for vasoactive meds?
- These lines end in the superior vena cava. What’s right after the SVC? The right atria. The right atria has a bunch of blood in it.. Therefore, when these meds are given in a central line, they’re immediately diluted in a large amount of blood. So it’s the fact that the medication is immediately diluted with blood that makes it okay to give them in these lines, not the diameter of the catheter.
- What’s a lumen?
- See below picture, it is what is labeled as a “cap”
- There are typically 1-3 lumens
- You administer medication and draw labs from these lumens
- These lumen should have caps on them, which create a one-way valve so that blood can’t leak out and bacteria can’t creep in
- You must clean these like CRAZY every time you use them
- “Scrub the hub” – meaning, clean the cap 10x over with an alcohol swab
- Joint Commission’s informational flyer on how to “Scrub the Hub”
- KNOW YOUR HOSPITAL’S POLICY. Seriously. Know this inside and out.
- You must check and see blood return with each use
- If there is no blood return, that means a clot has formed on the end of the catheter and you can push fluid through, but because a clot is there, it’s preventing blood from being withdrawn.
- This is a major concern because the clot could dislodge and travel
- Do not use and call MD or follow existing policy when this happens
Care of CVC’s – everything is the nurse’s responsibility!
- Get rid of them as soon as we don’t need them , only get one if its really needed
- Look at the dressing frequent, change every 7 days – or per policy: increases chances of infection each time you remove the dressing
- Antimicrobial patches are frequently used at the insertion site
- Change caps with blood draws
- If it has gauze over the insertion site, look at your policy and see if you can change it before the 7 days… you can’t see the insertion site
- Clean hub.. scrub the hub ten times before access, letting it dry, or use caps..
When inserted, get all new lines.. don’t hook older tubing to a new central line - Educate patient and family
- Talk about infection risk and encourage them not to touch it at all
- Tell them to let you know if they start to have pain/tenderness or notice redness
- Discontinue per policy
- Lay patient FLAT! This is really important
- If you pull and meet resistance, stop!
- General IV stuff
- Label your tubing
- Know how often to change tubing
- Many are 72-96 hours if continuous and 24 hours if not continuous
- Change tubing and fluid bags before shift change if needed
- It is courteous to make sure your patient has good tubing and full bags before shift change
Additional references and resources
- How to Keep Calm and Prioritize when Things Go Nuts
- How to Become an ICU Nurse
- Lippincott NursingCenter: Central venous access devices
- Webster J, Osborne S, Rickard C, Hall J. Clinically-indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2010;(3):CD007798. [go to PubMed]
- Lee WL, Liao SF, Lee WC, Huang CH, Fang CT. Soft tissue infections related to peripheral intravenous catheters in hospitalised patients: a case-control study. J Hosp Infect. 2010;76:124-129. [go to PubMed]
- Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81:1159-1171. [go to PubMed]
- American Nurse Today: Providing optimal care for patients with central lines
Wish someone would just teach you the cardiac stuff that matters?

Cardiac nursing can feel like you're drowning in alarms, rhythms, and unfamiliar meds before you even get report—and you're expected to keep up. But here's the truth: you don’t need to know everything, you just need to know what matters most.
Cardiac Confidence was created by experienced nurses to help you cut through the noise. We cover what actually shows up in real life—like post-cath care, recognizing unstable rhythms, caring for chest tubes, and knowing when to escalate (and a lot more).
No fluff, no advanced cardiac stuff you don’t need yet. Just focused, foundational info that makes a big difference.
Start Lesson #1 Now




Hi,
I am enjoying your content so far! I’ve worked with CVCs before, but there’s a lot additional information that I didn’t have prior.
You’ve mentioned in this episode, towards the end, that you’d post in the show notes how to position a patient if an air embolism is suspected during/after CVC removal by the nurse. I did a quick google search, and is it truly the Left Side Lying + Trendelenburg position, to trap the air in the right ventricle, and prevent it from travelling further?
Thank you! 🙂
Hi!
I love FreshRN! I’m transitioning hospitals going from a med-surg/tele floor at one hospital to a telemetry floor at a different hospital, so I’m refreshing my new nurse brain.
I did want to ask about measuring PICC lines everyday to make sure that there is no swelling. Is that a policy you are familiar with?
Thank you for all the great content!
Hi Simmone! I have heard of that being part of policy before, but working in acute care in different health systems and units, that was never part of our policy. I know what’s crucial is that it’s being measured the same way every single time. I wouldn’t be surprised if this were part of policy, however but I don’t have any additional information to provide from my own personal experience unfortunately.