In the intricate world of healthcare, the shift change between nurses plays a critical role, ensuring the uninterrupted well-being of patients. Just like a flawless musical handover, a well-structured nursing report acts as the bridge, guaranteeing continuity of care.
This guide will equip you with the knowledge and strategies for how to give nursing report effectively. We’ll explore the essential elements of a comprehensive report, providing valuable insights to streamline the process and enhance patient outcomes. Let’s dive in.

Table of Contents
Introduction to Shift Reporting
Psst… Check out my podcast episode nursing report for newbies for more info on this 👇
The nurse report is a fast-paced information-sharing time between shifts. The off-going nurse reports off to the oncoming nurse in a systematic way.
Shift reports in nursing are vital for a seamless transition of care between nurses. This will allow you to quickly learn about each patient and what you need to do for the next shift (typically 12 hours). Here’s how they ensure three key things:
- Continuity of Care: By detailing a patient’s medical history, current condition, and treatment plan, the oncoming nurse gets a full picture. This allows them to pick up right where the outgoing nurse left off, avoiding delays or missed steps.
- Patient Safety: Shift reports highlight any potential risks or changes in a patient’s status. This early warning system helps the new nurse identify and address any concerns quickly, reducing the chance of complications.
- Effective Communication: Shift reports provide a structured way for nurses to exchange crucial information. This ensures everyone is on the same page, preventing misunderstandings and promoting collaboration that benefits the patient.
Different Types of Nursing Shift Report
Reports look different for different units – so your expectations should also be different.
- The ED is VERY focused on the specific problem at hand.
- The ICU report is extremely detailed.
- The floor is somewhere in between.
Therefore, if you’re in the ICU getting report from the ED, the report is going to be a lot shorter and more concise, focused on only a few key things and tasks.
If you are in the ICU and giving report to another ICU nurse, then you know report is going to take some time in order to ensure nothing falls through the cracks.
If you’re going to work in med surg, check out my Med-Surg Report Sheet article.
Preparation for the Nursing Handoff Report
Information Gathering
There is information you compile when writing down a report.
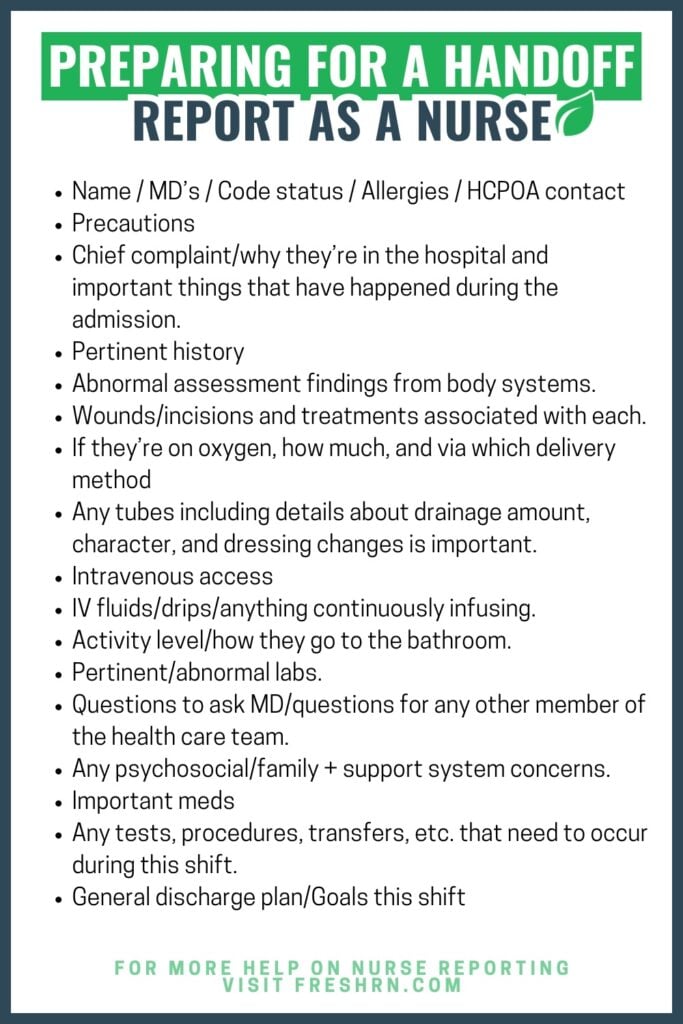
This is incredibly general and will vary if you’re on a specialized unit:
- Name / MD’s / Code status / Allergies / HCPOA contact info.
- Precautions (fall, seizure, infection prevention, bleeding, etc.).
- Chief complaint/why they’re in the hospital and important things that have happened during the admission.
- Pertinent history (it’ll take time to figure out what is pertinent or not, don’t get hung up on this one. You’ll also figure out, with time, shorthand/abbreviations for history).
- Abnormal assessment findings from body systems.
- Wounds/incisions and treatments associated with each.
- If they’re on oxygen, how much, and via which delivery method (nasal cannula, face mask, non-rebreather, etc.).
- Any tubes (feeding tubes, foley catheter, rectal tube, etc.), including details about drainage amount, character, and dressing changes is important.
- Intravenous access (IV, central line, port, etc.).
- IV fluids/drips/anything continuously infusing.
- Activity level/how they go to the bathroom.
- Pertinent/abnormal labs.
- Questions to ask MD/questions for any other member of the health care team.
- Any psychosocial/family + support system concerns.
- Important meds (you can look up this stuff in the chart, but they may mention some meds).
- Any tests, procedures, transfers, etc. that need to occur during this shift.
- General discharge plan/what are our goals this shift? (get out of bed 3 times, eat, pass swallow evaluation, transfer out of ICU, etc.).
Checklist Development
The fast-paced nature of healthcare can sometimes lead to crucial details being missed. Here’s where standardized checklists come in as powerful tools to streamline communication and guarantee a comprehensive handover.
Checklists empower nurses! They act as a safety net, minimizing errors by prompting a review of all essential aspects of a patient’s condition. This standardized format fosters clear communication between outgoing and incoming nurses, saving valuable time during shift changes. Ultimately, checklists enhance efficiency and contribute directly to improved patient safety by ensuring all critical information is exchanged.
How to Give Nursing Report – Structure of the Report
Clear and concise communication is the cornerstone of effective teamwork, especially in healthcare. It’s really important to review the chart while going through the report, so that means focusing on nursing orders – making sure things that should have been done are completed and all of your questions are answered.
- TIP! When deciding on a report sheet, give yourself some time with each sheet. You need to learn the sheet a little bit and where things are to see if it fits your needs.
- TIP! Approach it like a golf swing, do it the same way every time.
- TIP! Don’t get too focused on filling out each box in your report sheet. Patients are dynamic and different, so not every box may be necessary… and you may waste time trying to find irrelevant and/or unnecessary info just to fill every single one out.
- TIP! When giving shift change report to a nurse on the same unit, give report at the bedside. A lot of questions can be answered just by visually laying eyes on the patient. This also allows the patient to be part of the process. The more the patient is informed and included, the less questions and concerns they have because you are being transparent with them in the plan of care.
- Remember: the off-going nurse’s job is to paint a clinical picture, not ensure the oncoming nurse’s report sheet is filled out perfectly.
Critical Information First
Critical information about a patient’s condition or urgent needs should always come first. This ensures the oncoming nurse is immediately aware of any potential risks or areas requiring close attention.
Imagine a scenario where a patient experiences a sudden drop in oxygen saturation. Waiting until later in the report to mention this critical detail could lead to delays in intervention. By prioritizing critical information first, the nurse can immediately state: “Mr. Jones in room 205 is experiencing a rapid drop in oxygen saturation to 88%!” This grabs attention and allows for a swift response.
Critical information encompasses any urgent situation or change in a patient’s condition. This may include:
- Rapid changes in vital signs (blood pressure, heart rate, respiration, temperature).
- Sudden onset of pain or discomfort.
- Changes in mental status (confusion, drowsiness, agitation).
- Bleeding or unexpected drainage.
- Altered level of consciousness.
By prioritizing this critical information, you can establish a foundation for effective communication.
Nurse SBAR Report Sheet
Clear and concise communication is the cornerstone of effective teamwork, especially in healthcare. SBAR framework is a powerful tool that structures information exchange, promoting patient safety and improved outcomes.
SBAR stands for:
- Situation: This is a brief but critical statement that outlines the immediate issue or concern. Who is the patient? What is the current situation? For example: “I’m calling about Mr. Jones, room 205. His oxygen saturation has dropped to 88% in the past hour.”
- Background: Here, you provide relevant background information about the patient. This may include medical history, current medications, allergies, or recent procedures. Keep it focused on information pertinent to the situation. Continuing the example: “Mr. Jones has a history of COPD and is on oxygen therapy at 2 liters per nasal cannula.”
- Assessment: This is your professional judgment about the situation. What do your observations and findings suggest? Analyze the information and explain your interpretation. In our example: “Based on the drop in oxygen saturation, I’m concerned about potential respiratory distress.”
- Recommendation: Clearly state your proposed course of action. Do you recommend further assessment, intervention, or consultation? Be specific: “I recommend increasing Mr. Jones’ oxygen to 4 liters per nasal cannula and notifying Dr. Smith for further evaluation.”

How to Handle Orders Placed At or Around Shift Change
- Typically, if an order is placed at shift change, it’s the oncoming nurse’s responsibility to complete it. Nursing is a continual process, and while we’d like to pass our patients off all neat and tidy with everything done all the time, the reality is that doesn’t always happen.
- Remember, things happen at shift change, or things happen earlier and prevent the off-going nurse from being timely with everything.
- Have some grace and understanding, but also be able to verbalize when you think something should have been done.
- Talking point: “Hey if you could give that scheduled heparin that was due an hour ago before you leave, that’d be great. Thanks.”
Giving and receiving hand-off from an experienced nurse is pretty overwhelming to a nursing student or newly licensed nurse. In this previously released podcast episode, Kati and Elizabeth discuss:
- What nursing report is for an acute care nurse
- Unspoken nursing report etiquette
- Basics of what should be communicated during a normal full hand-off report
Effective Communication Skills
Clarity and Conciseness
The nursing shift change report is a time for the off-going nurse to share information and paint a clinical picture of the patient. It is an ineffective use of time to go through the chart and verbalize everything the oncoming nurse can just plainly see. Communicate the important things concisely, be clear to avoid misunderstandings, and describe the clinical picture.
Do you have a patient with frequent assessments ordered, such as neuro checks or neurovascular checks every hour or every 2 hours? Report is a great time to perform these at the bedside with the oncoming nurse (especially if the patient is coming from the ED or PACU). This way the ongoing nurse is seeing the same assessment as the off-going nurse. Doing this prevents a lot of confusion and can prevent an unwarranted call to the provider, especially if that facial droop is not new, but was not communicated during report to the oncoming nurse.
Utilizing a well-organized nursing report sheet for multiple patients ensures a smooth handover and clear communication between nurses.
Active Listening
Here are some tips on how to be an effective listener during a nursing shift report handoff:
- Be Present: Silence distractions, make eye contact, pay attention to detail, and minimize interruptions.
- Actively Engage: Ask clarifying questions, anticipate needs, and take organized notes.
- Solidify Understanding: Review the chart and visualize the patient’s condition.
Asking Questions
The person giving the report will go through their report and afterward, the person receiving the report asks questions.
- A “don’t be afraid to ask” culture is essential. Clarifying questions demonstrates your commitment to understanding the patient’s condition and promoting better care.
- “You mentioned Mr. Jones has a history of COPD. Can you elaborate on his current oxygen needs?”
- Don’t hesitate to ask questions if something seems unclear, incomplete, or contradicts your understanding of the patient’s medical history or current status.
- “You mentioned Mr. Jones is doing well, but he’s also on Lasix. Is there anything specific you’d like me to monitor regarding his heart failure today?”
- Do not ask questions to receive each piece of information. Allow the off-going nurse to give a full report, then ask clarifying questions. The report takes substantially longer if the off-going nurse is continually interrupted. Ask questions if you absolutely must during report, but try to save most for the end.
- Talking point: “Can you hold off questions until I’m done? I promise I’ll answer that.”
- Don’t be a jerk. If report was too concise or not comprehensive enough, don’t hate on the person. Same if there are tasks that weren’t done that you think should have been.
Use of Technology
Digital Tools and EMR
While a strong foundation in communication skills remains vital, electronic medical records (EMR) and digital tools are revolutionizing nursing shift reports. Here’s how technology streamlines the handoff process:
- They improve accuracy by providing easy access to crucial information and reduce errors by minimizing reliance on memory.
- Standardized reporting templates ensure consistent communication and clarity, while real-time updates guarantee the oncoming nurse has the most recent patient data.
- Integration with other digital tools allows for quick access to vital signs and medication details.
- EMRs foster collaboration by providing shared access to patient information for all involved healthcare providers.
Privacy Considerations
Nurses must treat all information, spoken or electronic, with utmost confidentiality:
- Disclose only details essential for patient care and avoid sharing unnecessary personal information.
- Be mindful of surroundings during verbal handoffs, choosing private areas to discuss patients.
- Utilize secure EMR systems, log out after use, and never share login credentials. Remember, strong passwords are essential.
Common Pitfalls and How to Avoid Them
Distractions and Interruptions
These are some strategies to minimize disruptions during handoffs:
- Schedule Dedicated Time: Block out a specific time for handoff reports, free from interruptions. This allows for focused communication and minimizes the risk of missed details.
- Find a Quiet Space: Conduct handoffs in a private location away from noisy areas or patient rooms. This ensures clarity and reduces the chance of misunderstandings.
- Silence Electronics: Put phones on silent and avoid checking emails or messages during handoff. The focus should be solely on the patient’s information.
- Standardize Handoff Procedures: Implement standardized protocols for handoffs, ensuring a consistent and efficient exchange of information that minimizes the potential for interruptions.
- Team Huddles: Conduct brief team huddles before handoffs to address urgent matters or questions, allowing for a more focused and uninterrupted handoff period.
Incomplete Information
A seemingly minor detail missing from a nursing handoff report can have a significant ripple effect, potentially impacting patient safety and overall care.
Incomplete information can lead to delayed interventions, increased error risks, misinterpretation, communication breakdowns, and negative patient outcomes.
Tips on how to ensure completeness:
- Standardized Tools: Utilize the SBAR (Situation, Background, Assessment, Recommendation) framework to ensure all crucial aspects of the patient’s condition are covered systematically.
- Checklists: Implement a standardized checklist to prompt nurses for essential information they might otherwise overlook during the report.
- Clarifying Questions: Encourage oncoming nurses to ask questions if anything seems unclear or incomplete. Don’t hesitate to seek clarification to ensure a full understanding of the patient’s situation.
- Review Documentation: Before the handoff, both outgoing and incoming nurses should review the patient’s chart to ensure they have a comprehensive picture of the medical history and current status.
Legal and Ethical Considerations
Documentation
Handoffs aren’t just about talking! Documentation is crucial for legal and ethical reasons. A clear and concise written record in the patient’s medical chart protects both the patient and the nurse. It ensures all important information is captured, minimizes errors, and demonstrates a commitment to ethical care.
This documentation typically includes the date, time, participants involved, patient information, key points about the patient’s condition, and any questions or clarifications discussed during the handoff.
Ethical Practices
Nursing handoffs are ethical tightropes. Nurses must balance clear communication with patient privacy. This means sharing only essential information, being honest and accurate, and advocating for the patient’s needs.
Objective reporting free from bias ensures a smooth transition of care, where the next nurse has a full understanding of the patient’s situation.
Role-Playing Scenarios and Examples
Practical Examples
Here are two scenarios to help you understand how to give nursing report with effective communication during handoff reports:
Scenario 1: The Stable Patient
Setting: Medical-Surgical Unit
Patient: Mrs. Jones, a 72-year-old woman admitted for a total knee replacement surgery two days ago.
Outgoing Nurse (Mary): Hi Sarah, I’m reporting on Mrs. Jones in room 205. She’s a 72-year-old post-op total knee replacement from two days ago. Pain is controlled with oral oxycodone 5mg every 6 hours as needed. She’s tolerating a regular diet and mobilizing with a walker, weight-bearing as tolerated. Her vital signs this morning were stable at 132/88, heart rate 78, respirations 16, and SpO2 98% on room air. She’s in good spirits and eager to go home soon. Is there anything specific you’d like to know?
Incoming Nurse (Sarah): Thanks Mary, that’s a great report. Did Mrs. Jones have any drainage from the surgical site?
Mary: Yes, minimal serous drainage noted on the last dressing change. The wound appears clean and intact.
Sarah: Perfect. I’ll be sure to assess the wound dressing during my initial assessment. Anything else to report?
Mary: Nope, that’s all I have. She seems to be doing well overall.
Scenario 2: The Unstable Patient
Setting: Emergency Department
Patient: Mr. Smith, a 55-year-old man with a history of COPD, who arrived by ambulance complaining of shortness of breath.
Outgoing Nurse (David): Hi Lisa, I’m reporting on Mr. Smith in room 3. He’s a 55-year-old with a history of COPD who came in by ambulance about an hour ago with shortness of breath. His oxygen saturation is currently 88% on a non-rebreather mask at 15 liters per minute. His vital signs are BP 140/90, heart rate 110, respirations 32, and SpO2 88% as mentioned. He’s using accessory muscles and appears in moderate respiratory distress. I’ve started him on albuterol nebulizer treatments and notified the doctor.
Incoming Nurse (Lisa): Thanks David, that sounds concerning. When was his last albuterol treatment?
David: Just five minutes ago. I’m planning to repeat it in 15 minutes if his oxygen saturation doesn’t improve.
Lisa: Okay, I’ll be sure to monitor his response closely. Did you get a chest x-ray?
David: Yes, it’s ordered and pending. I’ll let you know as soon as it’s available.
Feedback and Improvement
Don’t settle for just good handoffs! Strive for great ones through continuous improvement. Self-reflection and peer review can highlight areas for growth. Be openly comfortable with asking and providing feedback to other nurses regarding shift handoff practices.
Debriefing after shift changes helps identify communication gaps to make improvements. Ultimately, this translates to better patient safety, stronger collaboration, increased efficiency, and more empowered nursing practice.
Sample ED Nurse to Nurse Report
The Not-So-Secret Life of the Nursing Brain Sheet: Confessions of a Nurse’s BFF
Let’s face it, nurses have a lot to juggle. Medications, procedures, patient needs – it’s enough to make your head spin (and that’s before the caffeine wears off!). That’s where the trusty nurse brain sheet comes in. You might also hear it called a report sheet or, more affectionately, a nurse brain.
This little sheet of paper is a lifesaver. It’s like your memory’s best friend, capturing all the essential details about your patients during a shift. Think of it as a cheat sheet for grown-ups, filled with vital signs, meds, allergies, and all the quirky details that make each patient unique (like Mr. Smith’s fondness for polka-dot socks or Mrs. Johnson’s secret stash of crossword puzzles).
So, the next time you see a nurse clutching their brain sheet like a lifeline, remember – it’s not just a piece of paper. It’s a testament to their dedication, a silent guardian of patient information, and maybe, just maybe, a source of a little lighthearted humor during a busy day. Just don’t tell the head nurse you saw them using it as a napkin…
More Resources
End of Shift Report from Straight A Nursing
We also discuss giving and receiving report in all of our courses! To see the latest course catalog, click here.
Wrap-up!
Effective shift reporting is the secret sauce for seamless patient care. It’s a well-rehearsed performance where nurses rely on clear communication, active listening, and complete information.
Tools like SBAR and checklists keep things organized, while digital tools like EMRs add an efficiency boost when learning about how to give nursing report. But patient privacy remains the key melody – only share what directly benefits the patient’s care. Don’t forget the legal and ethical harmony – thorough documentation protects everyone.
The best part? This symphony is constantly improving. Nurses embrace feedback, hold debriefing sessions, and continuously learn to refine their communication skills. By fostering a culture of safety, open communication, and respect, nurses can ensure informative handoffs that translate to better patient outcomes, a smooth workflow, and an empowered nursing team. After all, effective communication is the beautiful melody that keeps the symphony of patient care playing perfectly.
Ready to learn more about how to take report nursing?
1. For a free mini-course on report tips for new nurses (including my fave report sheet), click here: https://courses.freshrn.com/p/med-surg-report-basics
2. To learn more about our comprehensive med-surg crash course, Med-Surg Mindset, click here: https://courses.freshrn.com/p/med-surg-mindset
3. Learn more about the FreshRN All-Access Pass, click here: https://www.freshrn.com/all\u2012access
Want to get ahead of the game and ease your anxiety about your first nursing job?

The FreshRN® New Nurse Master Class is the first-ever self-guided holistic nurse residency program. This comprehensive program was specifically created for the ambitious newly licensed acute care nurses who want to get ahead of them and build both their confidence and their clinical skills – all while learning how to adjust to the unique lifestyle of a nurse.
Want to stop feeling like an imposter in your first nursing job?

Your first nursing job is a huge milestone—but let’s be real, it can also be terrifying.
You’re expected to know so much, so fast—but what if you had a solid foundation before you even stepped onto the floor?
The FreshRN® New Nurse Master Class is the course we wish we had. It’s packed with the practical, real-world guidance
you need to feel more capable, confident, and in control.
From clinical skills and critical thinking, to time management
and self-care, this course covers everything they don’t teach you in nursing school—so you can feel ready, not just hope you are.
Start Lesson #1 Now



0 Comments