Surviving your first Code Blue or RRT can be stressful, but there are plenty of tips and resources you can use to survive during these emergencies. While first-hand experience is best, this is simply something that is lacking when you are a new nurse. So what can you do in the meantime to survive your first Code Blue or RRT?

About the Author

William Kelly, MSN, FNP-C is a Family Nurse Practitioner who runs Health And Willness, a nursing education blog that focuses on building clinical skills and knowledge for bedside nurses. Will has experience as a telemetry nurse, ER nurse, ER nurse practitioner, and inpatient hospitalist. He is passionate about using technology to better improve patient care.
- About the Author
- 1. Know When to Call It
- 2. Stay Organized During the Code Blue or RRT
- 3. Know your First-Line Treatments
- 4. Learn to Communicate Effectively
- 5. Assist in Nursing Care During Code Blue or RRT
- 6. Know Your Antidotes and Reversals
- 7. Know your Code Cart Medications
- 8. Get More Practice with Code Blues and RRTs
- 9. Seek Out Learning Opportunities
Want to listen to the podcast version of this post? Click play below! 👇
1. Know When to Call It
No – I’m not talking about when to call the code, as in stopping resuscitation efforts and calling the time of death. What I mean is: know when your patient is acutely decompensating and know when to activate the emergency response and call the RRT or Code Blue.
Code Blues tend to be a bit more straightforward. If the patient is not breathing or doesn’t have a pulse, start CPR and call a Code Blue to get the team there ASAP.
Rapid Response Teams, or RRTs, can be a little more tricky for the nurse to know when to “call an RRT”, and as a new nurse sometimes everything seems like an emergency!
Additionally, RRTs can be very stressful, even for experienced nurses, and we don’t want to err on the side of *pausion* (pausing when we need to act!).
There are many important reasons to contact the Provider or hospitalist team that may not require an RRT. Some non-emergent reasons to contact the Provider include:
- Pain medications
- Sleeping medication
- Clarifying an order
- Elevated blood pressure (otherwise asymptomatic)
- Breathing treatments (otherwise stable)
- Chest pain (if otherwise stable)
- Altered Mental status (otherwise stable)
Notice that the keyword is stable. Whenever the patient is in acute distress or their vital signs are significantly abnormal, this is when an RRT is needed. They aren’t coding yet, but if nothing is done ASAP, then they very well might code.
Reasons to call an RRT include:
- Respiratory failure with significant respiratory distress
- Unstable vital signs (low SPO2, Low blood pressure)
- Altered mental status when unstable or signs/symptoms of a stroke
- Hemorrhage (GI, epistaxis, etc)
- Cardiac Arrhythmias like sustained VTACH or rapid AFIB (typically rates >150)
In general, if the patient’s vital signs are unstable or if something is happening that will quickly make their vital signs unstable, you should call an RRT.
Clinical tip: Think to yourself “can this patient wait 20+ minutes for an evaluation and orders”. If the answer is no or you’re not sure – ask for help and/or call an RRT”.
2. Stay Organized During the Code Blue or RRT
This is half the battle of being a good nurse: staying organized and managing so many different moving parts. This becomes especially important when your patient crashes.
Calling a code or RRT means a team of experienced doctors, APPs, and nurses come rushing to help, and they’re going to have a lot of questions. As the primary nurse, it’s your job to relay the patient’s information in a concise and accurate manner. But we’re not perfect, and no one has a photographic memory like April Kepner on Grey’s Anatomy. This is why knowing WHERE to find all the information on your patient is crucial.
The first step in staying organized during your patient’s RRT or Code is to first get a good report from the previous nurse. This is difficult because it totally depends on that nurse’s ability to give a good report, as much as your ability to pay attention and write down the important information.
And speaking of, make sure you write down everything important. No – we don’t need to know everything they had for lunch – but make sure you write down things like:
- Major lab value abnormalities or trends
- Recent diagnostic results
- Important medications they’re on
- Locations of any IV sites
- Consults on board
Many facilities should have print-out sheets with a lot of this info already printed out. Becoming comfortable with these sheets (or making your own) is invaluable during times of stress. The more you know your sheet and how you organize it, the easier you will be able to find the information when it’s needed.
It is definitely helpful when you know the patient well and have taken care of them in the past. Keep your papers from previous days and/or keep the same one and update it!
3. Know your First-Line Treatments
After a while, RRTs and Code Blues become somewhat routine, at least in areas like the ER or ICU. On the Med-Surg floors though, it can take a few years before a nurse feels confident during a patient emergency because these emergencies don’t happen as frequently.
As the nurse, you or your colleagues on the floor are the first ones to notice something wrong with your patient and activate the rapid response. Once an RRT or Code Blue is called, it can take the team 5 minutes or longer to respond. This means it’s important to know the first-line treatments and initiate the ones you can.
For a Code Blue, one person should immediately start CPR and another person should get an AMBU bag and hook it up to 100% O2 (turn the oxygen all the way up) and start bagging the patient (Remember 30:2 until an advanced airway is established).

Another team member can quickly grab the code cart and hook the patient up to the defibrillator. If you find the patient alone, yell out for help while starting CPR, as compressions are always the priority during a Code Blue. If your facility has “Code Blue” buttons at the bedside, hit it!
For RRTs, if they are unstable you should still grab the code cart and at least wheel it outside the room. Always check vital signs when you can with every acute change. It’s never a bad idea to hook an unstable patient up to the defibrillator.
Here are some other interventions you can do as the primary nurse after an RRT/Code is called, but before the team gets there:
- All patients: Obtain Vitals, double check code status (i.e. are they DNR or DNI?)
- Coding Patient: CPR, Ambu bag at 100% O2 (30:2 compressions:breaths), hook up to defibrillator
- Hypoxic Patient: Titrate up their oxygen (will often require non-rebreather at 15L/min O2)
- Hypoglycemic patient: If unresponse, grab some IV Dextrose 50% (there is likely a protocol order if the patient is on insulin)
- Stroke Symptoms: Check a blood glucose and perform an NIH if possible, figure out last known well
- Syncopal Patient: Hang a bolus of fluid “at the ready”, hook up to cardiac monitor and/or defibrillator, get an EKG
- GI Hemorrhage: Get boluses ready to be hung ASAP, make sure the patient isn’t on blood thinners, make sure they’ve had a type and screen, get blood consent ready
- Unresponsive Patient: Sternal rub, check pupils, check a blood glucose, apply/check cardiac monitor
Always check their vital signs in a change of status. In general – do what you can to support their vital signs, and check blood glucose if the patient is altered.
4. Learn to Communicate Effectively
In order to effectively manage Code Blues and RRTs as a nurse, it is important to learn how to communicate effectively. This is important in all aspects of nursing and healthcare, as miscommunication can literally kill a patient.
During an emergency situation when the team gets there, they will need to know what is going on. You need to know how to accurately and concisely convey patient information in order for the team to make the right medical decisions.
These team members often are not familiar with the patient, so you are their best source of information. Sure, they can look up info in the chart on a computer on wheels, and they often do, however, this all takes time in an emergency, and time is not always a luxury.
One tool that I’ve created in order to give an effective report on a patient is the IMSBAR. Now, this really is just your standard SBAR but with some important clarifying information beforehand.
The first step is to give important information on the patient such as their name, age, and location. However, during an RRT, this often is not as necessary as everyone is already at the bedside and can see how old the patient is and does not really even need to know their name. This is more important over the phone.
The M stands for medical history and this is the medical history that is pertinent to the situation and/or their medical admission. You don’t want to list every medical history that they have, but list what is important.
For example, if a patient is hypoxic and in respiratory failure, be sure to include that the patient has a history of COPD, CHF, COVID-19, etc.
If the patient has chest pain, be sure to include if they have a history of CAD with stents, or any other cardiac or lung issue that may be related.
Then proceed with the typical SBAR format, listing the:
- Situation: Why did you call the RRT
- Background: Any relevant background such as any meds they are on, when their last breathing treatment was, etc.
- Assessment: Any relevant vital signs, what their lung sounds are, etc
- Recommendations: If you think you know what the problem is, say it, and if you have a possible recommendation – let the Provider know!
Example: “This is a 72-year-old male admitted for pneumonia with a history of COPD who developed severe respiratory distress suddenly, and their oxygen was 82% on 2 L nasal cannula. On a nonrebreather, they’re up to 94%. Their last breathing treatment was six hours ago and it was duoneb. Their lungs have wheezes bilaterally and they’re still breathing 36 times per minute. Do you want me to give another duoneb now?”
Learning to effectively communicate like this takes practice, and when you are nervous it is natural to fumble over your words as well as not remember typical stuff that you would when you’re not under so much pressure.
This is normal, but the more information you know and the better you practice communicating in this style, the easier it will be. This is the same style you can use while giving a report on a patient over the phone to a provider or another nurse.
5. Assist in Nursing Care During Code Blue or RRT
Just because a whole team of nurses and doctors are there to care for the patient, doesn’t mean you can’t help. Assist with any orders that are verbally given. This may include:
- Hanging fluid boluses
- Get an EKG
- Giving antibiotics
- Giving blood products
- Administering breathing treatments (often done by respiratory)
- Titrating oxygen devices
- Giving IV medications
As the primary nurse, you really shouldn’t be leaving the room until the RRT is cleared or the patient is transferred to a higher level of care. As you are the primary nurse, you know the patient the best, and you will likely need to answer any questions.
If something needs to be grabbed outside of the room such as in the med room or clean utility room, there are plenty of people who can go get that and be “runners”. Believe me, there will probably be people just waiting for something to do.
6. Know Your Antidotes and Reversals
Another important tip and becoming competent in emergency situations in the hospital is to know your antidotes and reversal therapies.
Now yes, these reversals should be ordered by the Provider, but it is definitely helpful to know these as the nurse.
Some important antidotes and reversals include;
- Coumadin: vitamin K, Kaycentra, FFP
- Heparin: Protamine sulfate
- Opioids: Narcan
- Benzodiazepines: Flumazenil
- Insulin: Glucose
- Hypercarbia: Bipap or intubation
- Tylenol OD: Acetylcysteine
- Digoxin: Digibind
- Anaphylactic Reaction: 50mg IV benadryl, 20mg IV pepcid, 125mg IV solumedrol, +/- 0.3mg Epinephrine IM
- Hyperkalemia: 10u IV insulin, 1-2 amps of D50%, 1gm Calcium Gluconate
7. Know your Code Cart Medications
The code cart is full of important medications that are literally life-saving. These are often required during an RRT or Code Blue. These medications include:
- Epinephrine
- Amiodarone
- Calcium Chloride
- Sodium Bicarb
- And more!
Many code carts will also stock D50, Narcan, and sometimes RSI medications.
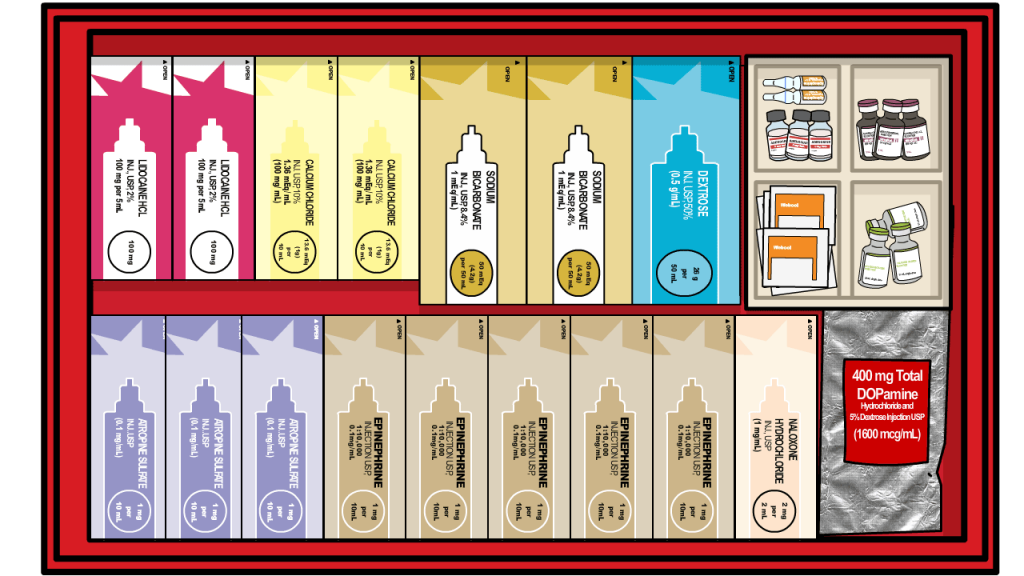
RSI stands for Rapid Sequence Intubation, and the medications used during RSI include paralytics and sedatives. These may not be stocked in the code cart, but rather in the Pyxis inside a kit (“the RSI kit”).
During a code or RRT, one of the nurses will typically choose or be assigned to the medication drawer. This is often the ICU nurse or an ER nurse, as they have much more experience with these medications.
It is important to know how to draw up these medications, as many of them need to be reconstituted, and quick mental math is not always easy when pressures are running high (sometimes literally… like 220/140 kinda high).
When you get free time, see if you can look at the medications in the Code Cart or RSI kit, how they are reconstituted, and how they are administered.
8. Get More Practice with Code Blues and RRTs
One sure-fire way to get better at RRTs and Code Blues is obtaining first-hand experience. The more RRT‘s and codes that you are actively participating in, the more comfortable you will be with similar emergent situations. Eventually, you’ll feel like you know what you’re doing!
It is normal to feel overwhelmed as a new nurse in these critical steaks situations where the patient’s lives are in the line. Do not beat yourself up over this, and know that you have done everything you can to prepare yourself for this moment.
At the end of the day, this experience will build upon your knowledge in order to help your future patient during a Code Blue or RRT.
If you can, respond to RRTs or Code Blues on other floors to help out, and get more experience. After all, it’s a little easier to learn when it’s not your patient who’s crashing!
9. Seek Out Learning Opportunities
Knowledge really is power, especially in the medical field. The more you know, the less you think you know, but the better the outcomes of your patient when you take that knowledge and put it into action, being a great bedside nurse.
One valuable tool you can leverage, especially as a new nurse, is your time! And what I mean by this is: spend your time seeking out additional learning opportunities to help you! You will not learn everything in nursing school. In fact, you’ll realize you really didn’t learn much at all compared to how much there is to know!
One of the important areas to focus on learning is patient emergencies such as RRTs and Code Blues. These are the situations that we are most at risk of not knowing what to do when the stakes are life or death. The team’s knowledge is directly put to the test, and we can see when we put that knowledge into action, it can dramatically improve the outcomes of our patients.
So how can you focus on learning more about managing a Code Blue or RRT as the nurse? Well for starters – you’re reading this article!
There are so many free and paid resources that you can use to improve your knowledge in these areas. Some examples of free resources include:
- Free Blog Posts (like the one you’re reading now and these:)
- Free websites and databases such as Wikem.org, FPnotebook.com, Medscape
- Nursing textbooks you already own
- Ask for tips from more experienced nurses
Some examples of paid resources include:
- ACLS and/or PALS (often paid for by your employment)
- Subscriptions such as UpToDate, Nursing Lexicon, Epocrates, etc
- Paid online courses
Online courses are created by knowledgeable nurses and healthcare workers who have been there on the front lines with first-hand experience and have done extensive research in the area. They then put that knowledge and experience into one digestible course to help you learn best!
Most online digital courses are affordable, and many times you can get CEU credit. You might even be able to use your continuing education credit with your full-time job to pay for these courses.
I have a digital course called the ECG Rhythm Master, which outlines every arrhythmia there is, how to identify them, as well as the treatment and nursing interventions that you should be doing for each cardiac arrhythmia. Learn more about that course below!
Additionally, FreshRN has ➡️ Cardiac Confidence ⬅️, which focuses on important cardiac pathophysiology, cardiac conditions, as well as other cardiac procedures needed for a cardiac nurse. This is super helpful for new CVICU nurses, but also important for ER nurses or just regular ICU nurses, or anybody who wants to improve their knowledge about the cardiac system and how that impacts bedside nursing.
And those are 9 Tips to Surviving Your first Nursing Code Blue or RRT. As you can see, a large part of being ready for a Code Blue or RRT is the proper organization, as well as effective communication and teamwork in saving the patient’s life and stabilizing their vital signs.
As with anything in medicine, hands-on experience is invaluable.
What was your first code blue or RRT? Did you know how to handle it? Did it make you have your own Code Brown? Let us know in the comments below.
Vitals & VibesWelcome to Vitals & Vibes—a series created just for new nurses navigating the real world of patient care – written by Kati Kleber, MSN RN. These quick reads are packed with practical tips, mindset shifts, and bedside wisdom to help you build confidence, one shift at a time. Whether you’re fresh off orientation…
Continue Reading PRN vs. Scheduled Meds: Quick Tips for Nursing Students
What does a “medical surgery nurse” do? Learn the correct spelling of “med-surg,” what it’s like to work on a medical-surgical unit, and why it’s one of the most important specialties in nursing.
Continue Reading Curious About a “Medical Surgery Nurse”? Let’s Talk Med-Surg
Let’s talk about what a med surg refresher course for new grad nurses should cover and ones to check out.
Continue Reading Med Surg Refresher Course for New Grad Nurses: What to Look For and #1 My Top Pick
Hate the ICU but still want to become a CRNA? Learn how to get into CRNA school with tips from an actual CRNA on ICU experience, prerequisites, interviews, and what it takes to thrive as a CRNA.
Continue Reading Hate the ICU but Eyeing CRNA? Here’s How to Get Into CRNA School (and Still Thrive)
AI in nursing predictions for 2026 reveal how nurse leaders expect technology to reduce burnout, support nurses, and restore patient connection.
Continue Reading AI in Nursing Predictions for 2026: What Nurse Leaders Say Is Coming Next
Understand the latest nurse liability claims trends from NSO, including high-risk settings like home health, corrections, and aesthetics, plus practical ways to reduce risk without practicing scared.
Report Should Never Feel Like A Pop Quiz 👇
This 30-minute mini masterclass teaches a simple, repeatable structure for giving and receiving med-surg report so you know what to listen for, what to write down, and how to speak up with calm confidence. No fluff. Just practical training you can use on your very next shift.
Unlock Instant Access for $27






0 Comments