Step into the world of critical care, where every beep, hum, and flicker of light provides life-saving information. As an ICU nurse, your mastery of common ICU equipment is pivotal. In this guide, we’ll delve into the cornerstone machines that drive the intensive care unit. Join us as we explore the tools that ICU nurses rely on daily in the world of critical care medicine.

Table of Contents for Common ICU Equipment
Important Perspectives and Definitions of Common ICU Equipment
In this post, we’re going to outline common ICU equipment that is used every single day in the critical care unit in a hospital. We are going to discuss these from the perspective of the nursing staff. Nurses are responsible for managing most of these vital tools, with some requiring additional expertise from the care team (respiratory therapists, ultrasound techs, code team nurses, pharmacists, and more).
You will soon learn that critical care medicine is unlike any other, specifically due to the high-alert medications and very serious equipment we must become experts at managing. This post will provide foundational knowledge about these important intensive care unit devices to get you started on the right foot.
Please note: Protocols and official procedures will vary from health care facility to health care facility. This post is informational as you learn more about the intricacies of patient care, and should supplement, not replace your knowledge.
Common ICU Equipment: Ventilators – The Breath of Life
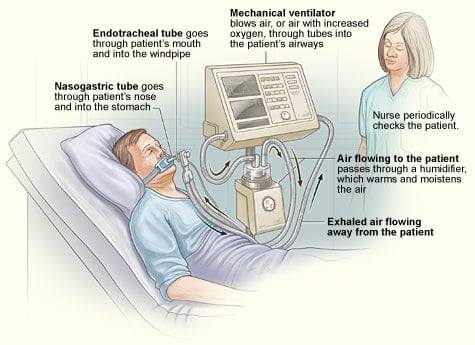
Description ➡️ Ventilators are the unsung heroes of the ICU, providing mechanical ventilation for patients who can’t adequately breathe on their own. These are likely the most common ICU equipment you’ll see on a day to day basis, along with the IV pump. These are often referred to as a “breathing tube” by laypeople. When people think of life support equipment, they most often are referring to ventilators.
Ventilators regulate air pressure, oxygen levels, and even the rate and depth of each breath. There are different modes that are customized to the patient’s respiratory needs.
Ventilators are attached to an endotracheal tube (ETT) or a tracheostomy tube, which is how the carefully programed breaths and supporting pressure levels are delivered to the lungs 🫁 through a flexible tube. Labs 🩸 are often drawn to complete the respiratory aspect of the clinical picture, specifically arterial blood gases (ABGs). ABGs measure things like the pH, partial pressure of oxygen, partial pressure of carbon dioxide, bicarbonate, lactate, oxygen saturation, and more.
Patients on a ventilator in the critical care unit are referred to as being “intubated” and the process of removing ventilator support is called “extubation”. For example, if the intensivist (ICU doctor) wants the ventilator removed on your patient, he or she may say something like, “Okay, let’s plan to extubate around 1100 today. Please notify respiratory.”
Tips for ICU Nurses with Ventilators
- Familiarize yourself with the various modes (assist-control, pressure support, etc.)
- Be vigilant for any signs of distress or discomfort in your patient
- Learn what the alarms 📣 mean; some require a very quick fix while others are more serious
- Your ICU respiratory therapist (RT) is a wealth of knowledge, so make sure you develop a good relationship with them and give them the green light to educate you on what they’re doing and why
Common ICU Equipment: ICU Bedside Patient Monitors – Guardians of Vital Signs
Description ➡️ Monitors are your eyes and ears, providing real-time data on heart rate, blood pressure, oxygen saturation, and more. They’re the first to alert you to any changes in a patient’s condition.
These machines are above to the patient’s hospital bed and are connected to the patient directly. They are also considered common ICU equipment. There will be a monitor in the patient’s room above their head as well as at the nurse’s station so that you can see it in both places.
These provide constant monitoring of vital signs and are necessary for both patients with life support and those without. These can include the heart rate, blood pressure (arterial and non-invasive), respiratory rate, and temperature (if an internal monitor is being used). Other data points can also be tracked but are not quite as common on every ICU patient (CVP, ICP, and more).
Tips for ICU Nurses with Bedside Monitors
- Customize your alarms to suit your patient’s needs and set appropriate thresholds; this should be done with each new admission
- Investigate the cause when the readings are inaccurate (blood pressure cuff slipped off the arm, telemetry lead stuck to the gown and not the chest, sweat causing the leads to come off, etc) to prevent alarm fatigue 😅
- Adjust alarm parameters when clinically appropriate for your patient (if your patient’s baseline heart rate is 40-50, but your monitor is set to alarm every time it goes below 50, consider switching the alarm to go off whenever the heart rate is low enough to necessitate action – which could be less than 40 in this scenario)

This is a bedside monitor. The top green line is the electrical activity of their heart and their heart rate, the second number (blue) is the oxygen saturation, and red numbers are the blood pressure.
This example is from neonatal ICU, but the set-up for adult ICU is essentially the same. You can change the colors of different numbers/lines as well. People tend to stick with the pre-set colors, but will change them if multiple other data points are added. For example, if I were the nurse for that patient, I would change the bottom color to something different, like yellow. If it’s an adult ICU, typically the bottom number is yellow and indicates the respiratory rate.
Common ICU Equipment: IV Pumps – Precision in Every Drop
Description ➡️ Infusion pumps deliver medications, fluids, and blood products with unparalleled accuracy. They play a crucial role in maintaining stable hemodynamics and delivering life-saving medications. There are different brands of pumps that all run differently that will require specific training to use. Alaris, B. Braun, Maxter, and Medtronic are some examples. If you want to be an expert in common ICU equipment, this is one to master STAT!
Medications are given from either an IV bag or a syringe and this travels through the tubing at a pre-determined rate, which is programmed into the pump by a nurse. When syringes are used, you may hear them referred to as “syringe pumps”.
IV pumps have special tubing that is used to deliver the medication into the patient’s blood stream, most often through a peripheral IV, or also through a central venous catheter.
Tips for ICU Nurses for IV Pumps
- Triple-check your settings, especially when you assume care for a patient with medication already infusing (a pump you didn’t set up yourself)
- Be vigilant for any signs of infiltration
- Pay attention to managing your ICU drips closely and accurately
- Always check compatibility before giving two meds in the same line

Top Meds Given in the ICU Through an IV Pump
In critical care, patients may receive a variety of medications through IV infusion pumps / syringe pumps to ensure precise dosing and continuous delivery. Here is a list of some of the most common medications administered through IV infusion pumps in the ICU:
- Normal Saline (0.9% NaCl): Used for fluid resuscitation and to maintain electrolyte balance.
- Ringer’s Lactate (Lactated Ringer’s Solution): Provides electrolytes and can be used for fluid resuscitation.
- Dextrose Solutions (e.g., D5W, D10W): Provides glucose and may be used for energy support or to dilute other medications.
- Potassium Chloride (KCl): Supplemented to maintain or correct potassium levels and when given IV, this is highly diluted.
- Insulin Infusion: Used for tight glucose control in patients with diabetes or those experiencing hyperglycemia.
- Propofol: A sedative-hypnotic used for short-term sedation in mechanically ventilated patients.
- Midazolam (Versed): A sedative and anxiolytic often used for sedation in critically ill patients. This can also be used in the neuro ICU for seizures.
- Fentanyl: An opioid analgesic used for pain control in ICU patients.
- Morphine Sulfate: Another opioid analgesic used for pain control in critically ill patients.
- Dopamine, Norepinephrine, Epinephrine: These are vasopressors/inotropes used to support blood pressure in patients with shock.
- Nitroglycerin: Used for vasodilation in conditions like acute coronary syndromes or hypertensive emergencies. This is most commonly given in cardiac ICU.
- Milrinone: A phosphodiesterase inhibitor used for inotropic support in heart failure or other cardiac conditions.
- Vasopressin: Used as a vasopressor in certain types of shock.
- Heparin or Enoxaparin: Used for anticoagulation in patients at risk for blood clots.
- Pantoprazole or Famotidine: Proton pump inhibitors or H2 blockers used for stress ulcer prophylaxis.
- Vancomycin: An antibiotic used to treat bacterial infections, especially those caused by Methicillin-Resistant Staphylococcus Aureus (MRSA).
- Cefepime, Meropenem, Piperacillin/Tazobactam: Broad-spectrum antibiotics used for serious infections.
- Furosemide (Lasix): A diuretic used for managing fluid overload or hypertension.
- Acetylcysteine: Used for acetaminophen overdose or as a mucolytic in conditions like COPD.
- Heparin Flushes: Used to maintain patency of IV lines and prevent clotting.
- Esmolol: A short-acting beta-blocker used for rate control in certain cardiac conditions.
- Amiodarone: Used for arrhythmia management, especially in ventricular tachycardia or fibrillation.
- Sodium Bicarbonate: Used to correct acid-base imbalances, especially in cases of metabolic acidosis.
Please note that this list is not exhaustive, and specific medications administered in the ICU can vary widely depending on the patient’s diagnosis, comorbidities, and individualized treatment plan. Always follow institutional protocols and consult with the healthcare team for specific medication management. While knowing the common ICU equipment is vital, knowing the meds is just as important.
Common ICU Equipment: Defibrillators – Shocking the Heart Back to Rhythm
Description ➡️ Defibrillators are the last line of defense against life-threatening cardiac 🫀 rhythms. They deliver a controlled electric ⚡️ shock to reset the heart’s rhythm. They are able to do this because the device can read the electrical activity of the patient’s heart. Pads are placed on the patient, an energy level is selected (this depends on the situation), and a shock is delivered to the patient. Defibrillators can both shock a patient’s heart and also provides cardiac monitoring during urgent/emergent situations.
Unlike the previous common ICU equipment discussed, defibrillators are not routinely hooked to patients. These are only used in a code (cardiac arrest) or during other specific cardiac situations.
Tips for Nurses with Defibrillators
- Ensure the pads are placed correctly
- Double-check energy levels
- Be prepared for potential adverse effects
- If you use this on a patient and they stabilize but you are still concerned, leave the pads in place for a few hours just in case they code again
- If you’re new to your unit, make sure you observe how these are used first
- Verify Patient Safety ➡️ Ensure there are no flammable materials near the patient, and that the patient is not in contact with any conductive surfaces (e.g., metal bed frame)
- Ensure Everyone is Clear ➡️ Before delivering a shock, ensure that everyone is clear of the patient and has ceased touching the patient or the bed
- If using for CPR ➡️ Begin chest compressions immediately after delivering a shock, following current guidelines for high-quality CPR.
- Defibrillators are located in your code cart

Common ICU Equipment: Ultrasound Machines – Seeing Beyond the Surface
Description ➡️ Ultrasound machines offer a window into the patient’s anatomy, aiding in procedures, assessing fluid status, and guiding the placement of invasive lines. A machine is used to bounce sound waves off of structures in the body and an image is produced. The sounds can also be heard audibly, which is helpful in determining blood flow.
While you won’t use these every shift, they would fall under the category of common ICU equipment without a doubt. Many of us are familiar with ultrasounds used to assess the baby of a pregnant woman, however these are used in many other clinical situations.
These machines are operated by physicians and ultrasound technicians, as well as nurses who are trained to use them. They can be very detailed or more basic. Naturally, the more detailed and complex images and data is obtained by ultrasound technicians. The more basic ultrasound machines can be used to aid nurses in the insertion of IVs.
Ultrasounds are painless and a gel is used between the probe and the patient’s skin, which will need to be wiped off when the examination is completed.
Tips for Nurses with Ultrasound Machines
- Familiarize yourself with basic ultrasound techniques and situations that would necessitate an ultrasound
- Collaborate with the radiology team for more advanced scans – like echocardiograms
- You won’t do the echocardiogram yourself, but you may need to assist with a bubble study 🫧
- Know your responsibilities in assisting physicians when they are using ultrasound for things like central line and arterial line placement (they are sterile for these procedures and you will help them)
- Familiarize yourself with expected normal results from ultrasounds and when to be concerned (normal ejection fraction, normal transcranial doppler readings, etc.)

The above image shows three examples of ultrasound machines. The image on the left shows the machine used by ultrasound technicians and the detailed images that are obtained. The upper right image shows the probe that placed on the patient’s skin. The bottom right is a handheld doppler ultrasound machine used by a nurse to detect a pulse. These are used in situations where a pulse might not be able to be palpated, but still could be present. The “125” on the screen represents the heart rate.
Common ICU Equipment: Hemodialysis Machines – Filtering Life
Description ➡️ Hemodialysis machines are lifelines for patients with kidney failure. They filter waste products from the blood, maintaining electrolyte balance. These may be referred to as a “dialysis machine” by patients and/or loved ones. A special tube is used to connect these devices to the patient, often referred to as a “dialysis catheter” that must be inserted by a specialist (this isn’t something a nurse does) directly into the blood vessels.
There are two types of hemodialysis machines: A continuous renal replacement (CRRT) and intermittent hemodialysis. There is a third type, peritoneal dialysis (PD), however this is most often used in the pediatric patient population and studies evaluating PD vs. CRRT in the adult ICU population showed CRRT to be much more effective and have a significantly lower mortality rate.
Intermittent dialysis is often performed by a dialysis staff nurse in the room of the ICU. Therefore, as an ICU nurse you would be responsible for care of the patient but not administration of the dialysis and use of the machine. However, because of the fluid shifts that occur, this type of dialysis might not be best for all ICU patients. Some cannot handle those changes and need something gentler that doesn’t produce such large swings in their hemodynamic status.
Continuous renal replacement therapy is different. As you can tell by the name, it’s continuous. And this can be a better option for the patient. This machine is operate by the ICU nurse. Patients who required CRRT are often very sick, and operating this machine takes their care up a notch in complexity. To be able to run one of these machines as an ICU nurse, you will need to take an additional training course. This is not a skill for new ICU nurses.
While not every patient will require this specific piece of common ICU equipment, many will. It will also be very important to detect the signs that dialysis is necessary.
Tips for Nurses with Hemodialysis
- Monitor closely for signs of hypotension and hypoglycemia
- Understand the anticoagulation protocol for CRRT. Monitor activated partial thromboplastin time (aPTT) or other relevant parameters as per protocol.
- Frequent Lab Monitoring: Check electrolytes, blood gases, and other relevant labs as per protocol. Adjust CRRT parameters based on results.
- Prevent Complications: Monitor for potential complications such as circuit clotting, air embolism, or access site infection.
- Prevent Hypothermia: Patients on CRRT may be at risk for hypothermia due to exposure to room-temperature replacement fluids. Keep the patient warm.
Medications Impacted by Hemodialysis
Hemodialysis can have a significant impact on the pharmacokinetics of certain medications. Medications that are water-soluble, have a low volume of distribution, and are not protein-bound are more likely to be affected by hemodialysis. Here are some examples of medications that may be impacted if given right before hemodialysis:
- Aminoglycoside Antibiotics (e.g., Gentamicin, Tobramycin): These drugs have a low volume of distribution and are primarily eliminated by the kidneys. Hemodialysis can significantly reduce their levels.
- Lithium: Hemodialysis can be effective in removing lithium, which is primarily excreted by the kidneys.
- Vancomycin: Although it is not typically removed by hemodialysis, changes in volume of distribution due to fluid shifts during dialysis may affect its levels.
- Salicylates (e.g., Aspirin): These drugs are weakly acidic and can be partially removed by hemodialysis.
- Theophylline: Hemodialysis can remove theophylline, which has a low volume of distribution and is primarily eliminated by the kidneys.
- Phenobarbital: Hemodialysis can remove phenobarbital, especially in cases of overdose or toxicity.
- Valproic Acid: Hemodialysis can be effective in removing valproic acid, especially in cases of overdose or toxicity.
- Methylxanthines (e.g., Theobromine, Caffeine): These substances can be partially removed by hemodialysis.
It’s important to note that the timing of medication administration in relation to hemodialysis can be critical. Medications that are given just before dialysis may be effectively removed, potentially leading to sub-therapeutic levels. In such cases, alternative dosing strategies may be required.
Final Thoughts on Common ICU Equipment
While we discussed the most common ICU equipment, there is a lot more to cover. Different types of feeding tubes (nasogastric tubes, PEG tubs, gastronomy tubes) EKGs, chest tubes, tracheostomy tubes, different types of oxygen delivery devices, wound vacs (very helpful for excellent wound care), and more are all found in the intensive care unit. (We discuss all of these in my crash course for new ICU nurses.)
You have to start somewhere and there’s no shame in being a beginner. If this is all 100% new, I highly recommend really zeroing in on learning the patient monitor first, then the IV pumps. Once you are highly familiar with these two, you’ll have a solid foundation.
Remember, being an intensive care unit nurse means you’re not just a task-master; you’re a lifeline for those who need it most, providing constant care. Mastering the intricacies of common ICU equipment is a powerful tool in your arsenal. One of my favorite resources for critical care staff is the Society of Critical Care Medicine. They provide great education and resources (specifically, the SCCM Podcast).
In your capable hands, these machines become conduits of hope and healing. Embrace the responsibility, and know that you’re making a difference every single day. Stay curious, stay vigilant, and never underestimate the impact of your knowledge and compassion.
More Resources for New Intensive Care Unit Nurses
- Intensive Care Unit Devices – Part 1: FreshRN Podcast
- Intensive Care Unit Devices – Part 2: FreshRN Podcast
- Common ICU Admission Diagnoses
- Common ICU Medications
- Sepsis Protocol for Nurses
- New ICU Nurse Master List – Meds, Procedures, Skills, Diagnostics, and More
- 6 Essential Tracheostomy Care Steps: A Comprehensive Guide
- Society of Critical Care Medicine
Starting in the ICU? Let's make it way less overwhelming.

Landing your first ICU job is exciting—but also a lot. The fast pace, complex patients, and steep learning curve can feel overwhelming.
That’s why we created Breakthrough ICU. This FreshRN® course gives you the real-world, practical guidance you need to start strong. 💪
Instead of just surviving orientation, you’ll walk in prepared and ready to learn—so you can build confidence faster.
Start Lesson #1 Now



0 Comments