Knowing the difference between the right and wrong medications is crucial to preventing medical errors. It’s one of the many components of medication administration for nurses, which we’ll outline in a simple format perfect for nursing students completely new to learning about medications, also called drugs or meds, and hey, you can even call it pharmacology if you’re feeling fancy.
One of the major things you learn in nursing school is how to give medications. In this article, I’ll explain some nursing basics related to giving medication as a nurse. When I was in school, no one told me this stuff… it was just assumed we knew all of this. That knowledge gap is one of the reasons I started FreshRN. I don’t want you to be left in the dark. Most of your classmates don’t know an adverse drug event from a hole in the ground, by the end of this article,e you will.
So, let’s go over some medication administration basics for nursing students.

Medication Administration Basics for Nursing Students: Why These Meds?
One of the most important things to know is why your patient is taking these specific medications. So take a look at their diagnoses and their medical history to identify why they might be on them.
Also, if you’re looking up medications and can’t figure out why a medication was prescribed, never fear! Sometimes, patients take things for off-label use. So, don’t forget to take a peek at off-label uses for the medication before you freak out.
Typically, nursing students have to look up the meds that their patient is on the night before their shift. Therefore, you’re looking things up without physically seeing them.
Quick tip: if it’s something weird that you’ve never heard of or it mentions percentages of fluid… it’s probably some sort of intravenous (IV medication), whether it’s it’s continuously infused (a drip or IV fluids), a one-time dose quick (IV push), or a one-time longer dose (IV piggyback)
One of the most important medication administration basics for nursing students is simply knowing the differences in the routes. They seem straightforward, but get a little dicey when we get into different ways we can give intravenous meds. Let’s go!
Routes
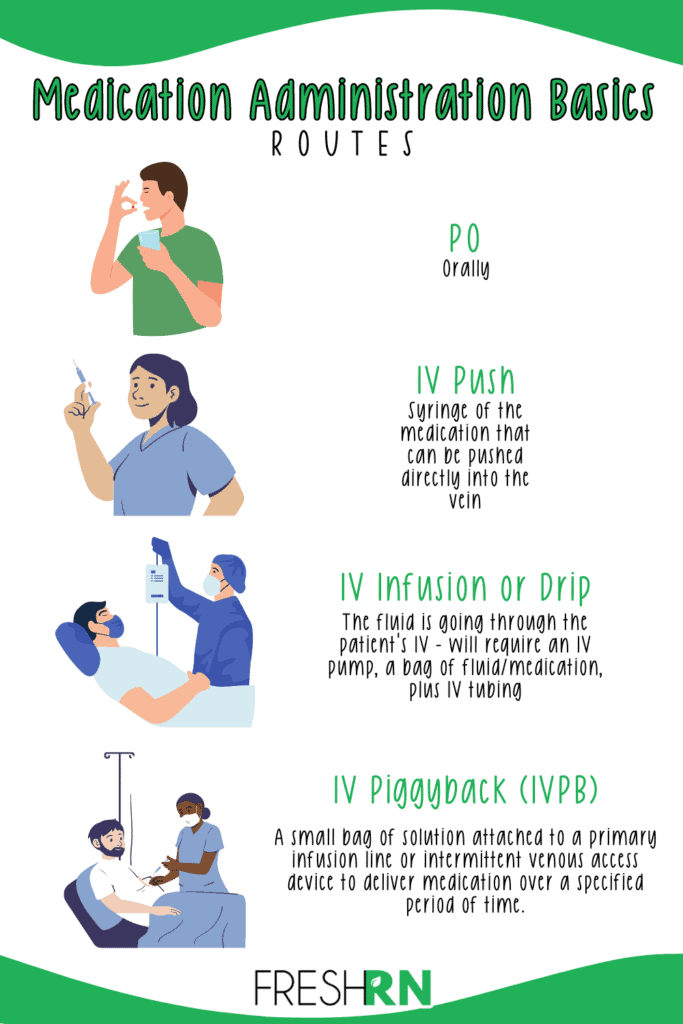
There are a few different ways you can give meds. These are the most common.. there are a few others that I won’t go into now because we’re talking basics.
(Note: We go over all of these in more detail in this FreshRN video course.)
PO
Orally. Easy enough, right?
IV Push (IVP)
IV push, meaning you have a syringe of the medication, and you push it directly in their vein. If you’re not sure how quickly you can push something, look at your medication reference guide. Most medications will be pushed around 1-2 minutes, but always check! Some are closer to 4-5 minutes.
Sometimes you must reconstitute (mix it up) with normal saline. These meds are in a vial, but in powder form. The package insert will tell you how much saline to use.
Most IV push meds are ones that are already in liquid form. You would draw up the correct amount of fluid (written on the order) to administer to the patient.
IV Infusion or Drip
IV infusion means the fluid is going through their IV. You will need an IV pump, a bag of fluid (or the medication), plus IV tubing to give this to a patient.
Your order should state the rate (how fast) the medication should go in (for example, 75 mL/hr) and how much is to be infused. It could say 75 mL/hr for 4 hours, or 75 mL/hr continuous, or a variation.
If the order says: 0.9% Normal Saline at 75 mL/hour, then you would:
- Get a set of primary tubing
- Get an IV pump
- One 10 mL saline fluid
- One 1000mL bag of 0.9% normal saline
Once you have your supplies, you’ll have to:
- Spike the bag with your tubing and prime it (to get all of the air out of the tubing)
- How you prime it depends on your IV pumps. Some will have you prime the tubing with a pump; some will have you do it before attaching it to the pump.
- Program your pump to infuse at 75 ml/hr
- Complete proper safety and identification checks
- Clean the hub and flush your patient’s IV with 10 mL of normal saline (or whatever the current policy is)
- Attach the primary tubing and press START
IV Piggyback (IVPB)
To administer something via IVPB means is different from the previous two. Imagine we’ve got a setup like I explained in the last section (continuous IV fluids).
The IV line connected from the large bag of fluids to the patient is called primary tubing. Meaning, it’s the tubing connected directly to the patient. On that primary tubing, there are two additional places where you can inject medications. These are called ports.
There is a port very close to the patient (called the Y-site) and another one very close to the bag of IV fluids that the tubing is spiked into near the top.
IVPB meds go into that port that is close to the top. The order means they want you to give another med (most often, an antibiotic) in the same line as the IV fluids, but they don’t want it to be the primary line. So you’re” piggybacking it” off of that one.
If the patient is getting normal saline at 75 mL/hr, and there is an order to give 3.375 grams of Zosyn at 60 mL/hr over 4 hours. You would need to get different tubing (called secondary tubing), attach it to the bag of Zosyn, and prime it (either on the pump or via gravity, whatever your hospital tells you to do).
Then, you’d program the pump appropriately and perform your safety checks. The pump will then stop giving normal saline at 75 mL/hr and give the Zosyn instead. Once the Zosyn is all done 4 hours later, the pump will automatically switch back to the normal saline at 75 mL/hr.
Transdermal
A transdermal patch is a medication patch that goes directly onto the skin. These patches are left on for hours or days at a time. They are very helpful to disperse medications slowly over a longer period, but they are not risk-free. It is imperative to document where you placed them and monitor the sites of patches that were placed before you took over for the patient. The last thing we want is to place multiple patches on the patient and cause an overdose.
With transdermal patches, you need to:
Choose the right location. You want it to be on a clean, dry, hairless skin area that’s not irritated or inflamed. Avoid frequently rubbed or stretched areas, such as the waistline, underwire bra area, or the back of the knee. Rotating the patch location with each application to prevent skin irritation is also important. The most common place is on the patient’s arm, right where you would give IM injections (the deltoid muscle, located at the top of the upper arm, just below the shoulder.)
Apply it appropriately. Remove the patch from its pouch and peel off half its protective liner. Place the adhesive side on the skin, then peel off the other half of the liner. Press the skin patch firmly with the palm of your hand for at least 30 seconds, ensuring it adheres to the skin, especially at the edges. (SOURCE)
Write on the patch. You should write the date and time you placed the patch on top. This helps people on the following shifts know when it was placed without having to look it up in the chart.
Leave the patch alone. If you touch the patch or attempt to relocate it, this can affect its adhesive properties and the release of the medication. Handle the patch by the edges or use gloves if necessary.
Document where it is. This helps subsequent shifts know where it is, when it was placed, and when to change it.
Important Note! Many patches stay on for days at a time. Therefore, the medication will be on your MAR, but you may not have a “due time” unless you place a new patch. You may have a task populated on your task list to remind you to check and document that the patch is in place and consistent with the last person who documented it. It is not your fault if the patient is NOT where the chart says it should be. Document where you found it; if you cannot find it, it may have fallen off. This isn’t a personal failure. It is an objective reality. Just tell the primary nurse or your clinical instructor, and they will get a new one placed. Transdermal patches falling off or getting misplaced happen, so don’t feel like this is a massive earth-shattering situation.
Throw it away appropriately. Dispose of used patches properly, following the manufacturer’s instructions or hospital policy. Some patches may need to be folded in half with the adhesive side together and flushed down the toilet, while others may need to be disposed of in a sharps container.
Sublingual
This means under the tongue. Again, not too bad! Make sure they don’t have gum, candy, or other things in their mouth. Sublingual nitroglycerin is the most common med given via this route. After giving a med like this, watch out for dizziness, hypotension, headaches, and nausea.
Per Rectum (PR)
Occasionally, you’ll need to give meds rectally. This can be done internally (inside the rectum) or needs to be applied externally on the anus.
The most common meds given internally are aspirin and acetaminophen. Make sure you use a water-soluble lubricant to coat the medication before insertion to ensure it goes in smoothly. You’ll want to educate the patient on what to expect since this is pretty uncomfortable and can be upsetting.
Intramuscular (IM) Injection
These are shots given in the arm or buttocks area. Most often, they are immunizations, but a few others are commonly given this route. You’ll give a lot of IM injections if you work in a pediatrics clinic, immunization clinic, or the emergency department.
These medications are often in vials, and you will draw the liquid up with a blunt needle into a syringe and attach a different needle to administer it to the patient. Some IM medications come in pre-drawn syringes.
The most common injection sites are:
- Deltoid
- Ventrogluteal
- Vastus lateralis
You’ll use the trusty Z-track method to administer these medications successfully. If you’re working in an ICU, med-surg, or similar unit, you will not give medications via IM very often.
Subcutaneous Injections (SUBCUT)
You will give subcut meds all the time. One of the most common ways to give insulin and heparin is subcutaneously. It is very effective and safe to give it via this route, so it is ordered often.
In clinical, you’ll give so many insulin injections that you’ll lose track after the first two weeks. It’s a smaller needle, and you pinch some skin in various approved areas and inject. It’s very simple but can be intimidating at first.
Compatibility
To dig deeper into medication administration basics for nursing students, let’s talk about an important aspect of safely giving IV meds. When you’re giving IV medications, ensuring everything is compatible is important. What does this mean?
When IV fluid is running, it is running through a primary line. So, the main fluids running are their primary IV fluids (normal saline, half normal saline, D5, D10, normal saline with potassium added, etc.). When you need to hang an IV antibiotic, you typically “piggyback” (hence the term IV piggyback) this onto your primary fluids, provided they are compatible. The antibiotic is then considered a secondary line. It is connected to the primary tubing. You set the pump to run your antibiotic at the prescribed rate, and it will (typically) automatically switch back to your maintenance fluids.
For example, if my patient has normal saline with 20 mEq of potassium chloride running at 75 ml/hr and I have a dose of Ancef due, I need to check to see if my normal saline with potassium chloride is compatible with Ancef. If it is not compatible, then I need to start another IV or if they have a PICC line (peripherally inserted central catheter), midline catheter, or central venous catheter, I have to use a different port.
However, please make sure to follow your hospital’s policy because some require people to have a dedicated line just for antibiotics (typically called a “med line”) rather than piggybacking it to a maintenance line.
Another thing to consider is if the maintenance fluid can be paused to administer the antibiotic. Think to yourself, do I want this paused for the duration of that antibiotic? Is that okay? If you have someone on an insulin drip and you’re piggy-backing Zosyn (which can take 4 hours to infuse) on their only dextrose source (maybe they have D5 at 50 mL/hr going), you’re going to have a mess on your hands.
I typically only piggyback things to maintenance fluids like normal saline.
To Crush or Not to Crush
You will encounter many patients who cannot swallow whole pills. This is typically due to impaired swallowing (strokes are a common reason). I don’t mean to brag, but I am a fantastic applesauce mixologist and can get even the grumpiest patients to take their meds. However, before you crush medications, you must know if they can be crushed. If it is an extended-release med, chemo, or capsule.. do not crush it!
There are also some meds that, for whatever reason, cannot be crushed. Depending on the medication administration process at your hospital, your EMR may tell you when you can and cannot crush your med. However, you must be diligent before crushing and double-check before doing so.
If you are unsure, call the pharmacy and ask to speak to a pharmacist and ask. There have been multiple times where I had a med that I knew I couldn’t crush, but the patient couldn’t swallow pills, so I chatted with the pharmacy, who either advised switching it to IV or something else (and called the physician for me to get the appropriate order!).
Avoiding Adverse Drug Events
As a nursing student, it is vital to understand the importance of avoiding adverse drug events (ADEs) to ensure the safety and well-being of your patients. An ADE can lead to significant harm, causing complications in the patient’s health and potentially leading to prolonged hospitalization or, in severe cases, life-threatening situations. This not only impacts the patient but also deeply affects their families, who may experience emotional distress and a loss of trust in the healthcare system. Beyond patient care, ADEs can have serious implications for your future as a nurse. They can lead to legal consequences and professional disciplinary actions, jeopardizing your nursing license and career reputation.
These events also reflect poorly on the healthcare facilities, possibly leading to financial penalties and a decline in the perceived quality of care. As you progress through your nursing education, it’s crucial to focus on accurate medication management, understanding the interactions and effects of various drugs, and maintaining meticulous attention to drug administration. This knowledge is essential not just for your professional growth. Still, it is fundamentally important to protect and maintain the trust of patients and their families in your care and the healthcare system at large.
6 Rights of Medication Administration

The foundational aspect of medication administration basics for nursing students are the six rights of medication administration. The rights of medication administration refer to a set of principles that nurses and nursing students should follow when administering medication to patients. These principles aim to ensure that patients receive safe and effective medication and minimize the risk of medication errors.
The six rights of medication administration are:
- Right patient: The nurse must ensure they administer the medication to the correct patient. This involves verifying the patient’s identity using two identifiers: their name and date of birth.
- Right medication: The nurse must ensure they administer the correct medication to the patient. This involves checking the medication label against the medication order or prescription.
- Right dose: The nurse must ensure that they are administering the correct dose of medication to the patient. This involves calculating the correct dose based on the patient’s weight, age, and other factors and verifying the dose against the medication order or prescription.
- Right route: The nurse must ensure that they administer the medication by the correct route (mentioned before). This involves following the medication order or prescription and checking that the route is appropriate for the medication and the patient’s condition.
- Right time: The nurse must ensure that they are administering the medication at the correct time, according to the medication order or prescription. This involves checking the patient’s medication schedule and administering the medication at the appropriate interval.
- Right documentation: The nurse must document the medication administration accurately and completely. This involves recording the medication name, dose, route, time, and other relevant information in the patient’s medical record.
Following the six medication administration rights helps ensure patient safety and minimize the risk of medication errors. Nurses must also be aware of any potential drug interactions, adverse effects, or contraindications associated with the medication they are administering and take appropriate precautions.
Overwhelmed?
There are so many medication administration basics for nursing students to learn, but don’t lose hope! No one expects you to know all of the medications ever made, their dosages, interactions, trade and generic names, etc.
You’re just building the medication foundation right now – and you’re not just building a house, you’re building a skyscraper.
When you get out of school and start your first job, you will get very used to the medications you give day in and day out. You will learn them inside and out. If you’re a cardiac nurse, you will know Amiodarone, Lopressor, Cardizem, and Epinephrine. If you’re an L&D nurse, you’ll know Pitocin and Magnesium. If you’re a neuro nurse, you’ll be rocking 3% saline, Mannitol, and Keppra. Once you know what you need to focus on, I promise it will get much easier.
If you’d like me to walk you through the basics of medication administration together with another experienced nurse, check out the FreshRN Nursing School Clinical Prep course below!
Medication Administration Basics for Nursing Students: More Resources
- Pharmacology Tips for Nursing Students – From a Nurse!
- 3 Pharmacology Tips to Help You Pass the NCLEX
- How to Survive Nursing School Masterpost
- Nursing School Math Exams
- What is the Difference Between Nursing Externships and Internships?
Feel like nursing school didn’t prepare you for clinicals?

Nursing clinicals are awkward at first. You’re surrounded by experienced nurses, real patients, and you’re just trying to figure out where the gloves are. It’s a lot.
That’s why we created Nursing Skills Refresh—to give you a realistic, supportive head start. You’ll get demo videos of common procedures, insider tips from two experienced nurses, and a clear picture of how a shift actually flows. (and a lot more) The goal? Walk into clinicals feeling like you belong there—not like you’re in the way.
Start Now



Hi, I’m loving your nursing blogs, especially for student nurses. I’m in my second semester of accelerated nursing school and taking Pharm along with starting our clinicals in a couple of weeks and passing out meds soon! I have a question about the NCLEX regarding pharmacology – how much do we need to do? Right now, Pharm is SO much info, and I feel overwhelmed trying to figure out what exactly I need for the NCLEX.
I just added a link to a resource that I’ve found incredibly helpful since I last updated this post in 2015. It’s a self-guided virtual pharmacology course that really breaks things down in the most concise way possible. The basics you need to know to how to physically administer meds is covered here, but a course like that will go into the other side of meds: the mechanism of action, things to watch out for, disease processes they work on specifically, and so forth. If you are able to understand the mechanism of action and different classes – that’s super important!