Nursing assessments are fundamental in your day-to-day in your responsibilities. You must understand what’s going on with the patient at the beginning of your time with them so that you can know whether or not that has changed over time.
The ICU, ED, floor, PACU, and other units have different assessment processes and expectations. Two very common types of assessments are head-to-toe assessments and focused assessments.
Head-to-Toe Nursing Assessment
A head-to-toe assessment is a comprehensive nursing assessment that involves a thorough examination of a patient’s physical and psychosocial status. This type of assessment is typically performed at routine intervals on nursing units like intensive care, stepdown, and med-surg.
How Often Are Head-to-Toe Assessments Required?
If the patient is in critical care (CVICU, neuro ICU, ICU, transplant ICU etc.), hospital policy likely require a full head-to-toe assessment to be performed and documented at least every four (4) hours. If the patient is on a med-surg floor (or similar), policy likely requires a head-to-toe assessment to be performed at least once per shift, with change of care giver, or after an event/change in status (for example, after a rapid response call).
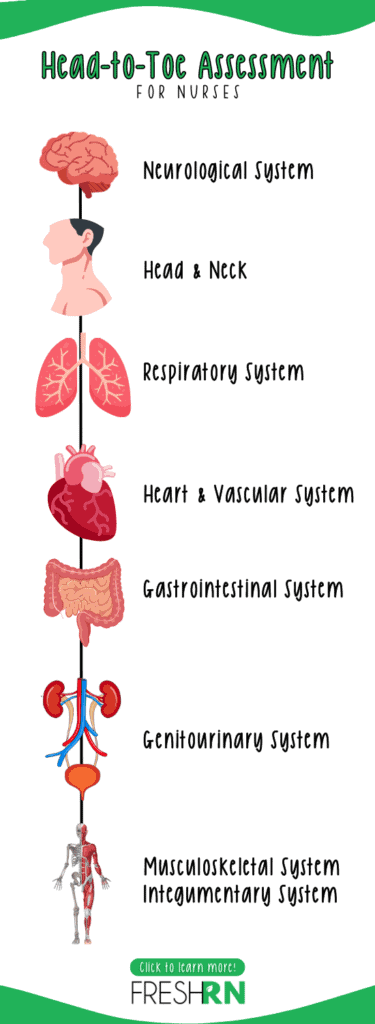
What is Included in a Head-to-Toe Assessment?
During a head-to-toe assessment, the nurse evaluates the patient’s overall health status by systematically examining each body system, from head to toe. It is important to move from head-to-toe, otherwise you can easily miss steps.
Pro-tip: It’s helpful for the nurse to be aware of abnormal assessment findings from the previous nurse prior to completing their head-to-toe assessment, as well as know penitent medical history and any current issues that could impact their findings to add context. The findings from the previous nurse are often communicated during nursing report. The remaining details are often found in the patient’s chart. Finally, it is helpful to know what the patient’s hemodynamic status is (most recent vital signs) prior to completing the assessment. All of these details help the nurse to establish a baseline for the patient’s health status, identify potential problems, and develop an appropriate care plan.
Neurological system
The nurse will assess the patient’s mental status, reflexes, and sensory function, as well as checking for any signs of neurological deficits.
I discuss full neuro assessments more in-depth here.
Head and neck
The nurse will assess the patient’s eyes, ears, nose, mouth, throat, and neck for any abnormalities or signs of illness. This includes checking for jugular vein distention, ensuring the mucous membranes are not dry or pale, that swallowing is not impaired.
Chest and lungs / respiratory system
The nurse will assess the patient’s respiratory status by listening to breath sounds, checking for chest expansion, and observing for any signs of respiratory distress and noting the work of breathing.
Knowing the patient’s oxygen saturation is helpful when assessing their respiratory status, as well as what their oxygen requirements are and if that has changed recently (for example, if they were only 2L nasal cannula for the last two days and now they’re on 5L to maintain the same oxygen saturation).
Heart and vascular system
The nurse will assess the patient’s heart rate, rhythm, and blood pressure, as well as checking for any signs of peripheral vascular disease. This includes listening to their heart sounds, checking for edema in their extremities, and assessing peripheral pulses (radial, dorsalis pedis, posterior tib).
I discuss cardiac assessments in depth here, and have a checklist you can download here.
Abdomen / gastrointestinal system
The nurse will assess the abdomen by first listening to bowel sounds in all four quadrants (here’s my fav stethoscope). Then, the nurse will palpate the abdomen and note any tenderness and inquire about recent bowel patterns and challenges.
Genitourinary system
The nurse will assess the patient’s urinary output, noting if the patient is voiding normally. Nurses do not routinely inspect the genitals unless it is specifically indicated (for example, if the patient recently had a urological procedure or has a urinary catheter in place). If the patient has voided, the nurse will assess the color, clarity, amount, and odor.
Musculoskeletal system
Throughout this head-to-toe assessment, the nurse will note the patient’s range of motion, muscle strength, and any signs of pain or discomfort. Often, nurses ask the patient to squeeze their hands and then instruct them to push and pull against them to note grip and bicep/tricep strength and if it is equal. They also often ask the patient to dorsi and plantar flex their feet to assess the lower extremities as well.
It’s helpful to note if the patient is ambulatory, and by observing the patient walk, that can tell the nurse quite a bit about the patient’s musculoskeletal system.
Integumentary system
Throughout this entire assessment, observe their skin. Note any color changes, impaired skin integrity, weeping wounds, and the status of any dressings. It is very important to assess bony prominences to ensure there isn’t any redness forming or already present pressure ulcers. This includes the coccyx.
Focused Nursing Assessment
A focused assessment is a type of nursing assessment that is used to gather information about a specific problem or concern related to a patient’s health status. Unlike a comprehensive assessment, which is a more thorough evaluation of the patient’s overall health status, a focused assessment is more targeted and limited to a specific area of concern.
For example, a focused assessment may be performed to evaluate a patient who is experiencing chest pain. The nurse will focus on gathering information about the chest pain, such as its onset, duration, and intensity, as well as any associated symptoms such as shortness of breath, nausea, or diaphoresis (sweating).
The nurse will also perform a physical examination to assess the patient’s cardiac function, including auscultating the heart and lungs, assessing vital signs, and checking for any signs of circulatory compromise.
Other examples of focused assessments include:
- Skin assessment: This may be done to evaluate a patient’s skin condition, including the presence of any wounds, rashes, or lesions.
- Pain assessment: This may be done to evaluate a patient’s pain level, including its intensity, location, and duration.
- Mobility assessment: This may be done to evaluate a patient’s ability to move around, including their range of motion, muscle strength, and any signs of discomfort or pain.
- Nutrition assessment: This may be done to evaluate a patient’s nutritional status, including their dietary intake, weight, and any signs of malnutrition.
A focused assessment helps the nurse to identify specific problems or concerns, develop an appropriate care plan, and monitor the patient’s progress. It is an important tool for providing patient-centered care and ensuring that patients receive the necessary interventions to address their individual needs.
Preparing for the Nursing Assessments
Some tools that may be useful during an assessment include:
- Penlight
- Vital sign supplies: blood pressure cuff (or automated machine), thermometer, pulse oximeter
- Stethoscope
- Handheld doppler – this is necessary if you cannot palpate pulses
Your nursing school textbook will mention things like an otoscope, tongue depressor, and more. However, in routine head-to-toe assessment and focused assessments, these tools are not necessary. If you work in highly specialized areas like labor and delivery, you may need other tools.
Non-verbal Cues: Just as Important
While much of a nursing assessment focuses on biological or physiological attributes and active listening, nurses also need to be able to pick up on certain non-verbal cues. Sometimes, what a patient doesn’t say is the most critical piece of information. Non-verbal cues can include:
- If the patient is purposefully moving all four extremities spontaneously
- If the patient able to complete basic tasks without help or cueing (getting a drink of water, turning on the TV, repositioning themselves in bed)
- Able to communicate with visitor and the nurse / staff with ease
- Discomfort speaking with specific individuals or about specific topics
- Indicators of pain while completing the assessment (wincing, clenching jaw, deep breathing, tense)
- Vital sign
Pay attention as you’re entering the room, before you begin your verbal interaction, and while you perform your assessment. Also, make sure to observe non-verbal cues throughout your shift.
Building Rapport
By establishing a trusting and professional relationship with your patient, your are building rapport. This enables your patient to relax and be honest with how they are feeling and what they are thinking which ultimately enables you to obtain a more accurate assessment, and thus better provide better care. You can do this by confidently introducing yourself at the beginning of your shift.
“Hi my name is Kati, and I’ll be your nurse today.” [extend hand for a handshake]
This is such a small gesture, but it makes a big difference to patients and loved ones.
Communication
Communicate clearly throughout the assessment with your patient. Ask before you start touching the patient, and explain what you are doing as you do it. My favorite talking point is:
“Alright, I need to look you over really quickly. Is it okay if I ask you a few questions, listen to heart and lungs, and all that jazz?”
(Insert witty comment from the patient here)
“Okay, can you tell me your name, what year it is, and where you are right now?” (Or some variation of orientation questions.)
“Alright, I’m just going to shine this pen light into your eyes for a moment while I look at your pupils. Focus on my nose.”
“Ok great, can you lean forward so I can listen to your lungs on your back? Okay great, give me some slow deep breaths.”
Documentation
Documentation is a critical part of the assessment process. This helps you download your findings from your brain to a reliable place (the patient’s chart) so that you do not need to struggle to remember it later on, and enables nurses on future shifts to know what the patient’s assessment looked like at specific times.
There have been many times as a bedside nurse in which I detect assessment changes, and immediately refer back to the chart to see what the previous nurse’s documentation showed. This is very helpful and enables you to gauge your level of urgency accordingly. Maybe you noticed what you thought was a change, but when you review documentation, it is clear that this is a known abnormality (and therefore likely does not require physician notification).
Final Thoughts on Nursing Assessments
These assessments may become routine to you, but are a one-off sometimes for patients. Having their private areas looked at, or asking personal questions can be a lot for some, so ensure that you are paying attention to their demeanor and being kind and caring.
Finally, do not underestimate the power of a quality assessment. This informs physicians in their decision-making, which can be life or death. Physicians see the patient for only a few minutes each day, but the nurse is who is there 24/7. The medical team is relying on your expertise to notify them when something changes.
My biggest tip for nursing assessments is to complete a solid assessment at the beginning of your shift so that later on if something changes, you have something to compare it to.
Godspeed, nurses and nursing students!
More Resources for Nursing Assessments
Feel like nursing school didn’t prepare you for clinicals?

Nursing clinicals are awkward at first. You’re surrounded by experienced nurses, real patients, and you’re just trying to figure out where the gloves are. It’s a lot.
That’s why we created Nursing Skills Refresh—to give you a realistic, supportive head start. You’ll get demo videos of common procedures, insider tips from two experienced nurses, and a clear picture of how a shift actually flows. (and a lot more) The goal? Walk into clinicals feeling like you belong there—not like you’re in the way.
Start Now



I would love to win the injector course!
This is a good overview of assessments. I’m getting more into wound care and the assessments are critical. So important to go down the list so nothing is missed.