First of all, I want any new nurses or students out there reading this to know: Learning how to do this is tough. It takes some time to understand how to interpret 5-Lead ECGs, and there are a lot of considerations. This is a complex nursing skill. Naturally, acute care cardiac nurses will deal with this much more than someone who works inpatient rehab, orthopedics, or on another non-cardiac unit. However, many patients are on some form of cardiac monitoring, so knowing the basics is a crucial step to functioning as a safe and competent nurse.
Table of Contents
Let’s dive into what acute care nurses need to know about 5-Lead EKG/ECG Interpretation so you can look like a pro! (And be way ahead of where I was as a student)
Note: While we’re chatting about 5-lead here, you could also run into 3 and 12-lead. We mention those later on, but they are not the focus of this article. When I mention “telemetry” I am referring to a 5-lead cardiac monitoring.
ECG vs EKG – what’s the difference?
Basically, an EKG is the exact same thing as an ECG. You’ll hear it called both, and they both mean electrocardiogram.
You may be wondering where that K comes from in EKG. Well, it originates from the German spelling of electrocardiogram (elektro-kardiographie). It’s a basic difference in spelling and language (like color vs. colour) and doesn’t change the meaning.
You can confidently use EKG and ECG interchangeably. You may run across people who are adamant one way or the other, but it’s nothing to get your telemetry leads all twisted up 😉
What’s an ECG telling us anyway?
📌 Real quick, would you prefer a handy reference instead of a whole blog post? Download my FREE ECG Interpretation Cheat Sheet (perfect for the floor or clinicals). ⬇️
Okay let’s get into it. It’s basically measuring the electrical activity of the heart. Why does the electrical activity of the heart matter, you ask? Well, the electrical activity is essentially what is telling the heart muscles to beat! Without a good, predictable and reliable signal, you cannot have an effective heart beat.
Without an effective heart beat, blood doesn’t get pumped appropriately throughout the body (the fancy term for this is “decreased cardiac output” because the heart isn’t pushing out the right amount of blood). Oxygenated blood provides the body the absolutely essential oxygen, so for this to be impaired, it’s a pretty big deal, and if severe enough, can cause life-altering consequences or even become fatal.
Ok, back to the electrical signal: It goes through a specific pathway through the heart, and then starts back up again. The electrical signal which causes the heart muscle to contract is what is you will see on your ECG monitor. To be able to continuously view this electrical activity, we have to use a heart monitor.
Heart monitor is very general term, and they can get very detailed. But basically, it uses electrodes (sticky pads) that connect to leads (look like thin phone charger cables), which connect to a box or a monitor. These leads are like little cameras, taking a continuous video of the electrical signal of the heart, and transcribing it on to the monitor.

(Note: If patients are in ICU, the emergency department, or stepdown, they likely have one that looks a little different. I explain that more in my mini course, ➡️ Telemetry Basics-Brush Up ⬅️.)
The electrical impulses are shown on the screen as a line with waves on it. The straight line means that there isn’t activity, and then when an impulse happens, we see a wave. The type of wave we see depends on where the impulse is located at that time. The impulse created by the atria is naturally much smaller than what’s created by the ventricles because, well, the atria are a lot smaller!
The normal steps it takes are:
- It starts in the Sinoatrial node (SA node), which is in the atria.
- The Atrioventricular node (AV node), which is located in between the atria and ventricles (hence the name)
- Bundle of His, which is located in the septum of the heart
- Bundle Branches, which is where the Bundle of His branches off farther down in the septum
- And the end of the line is the Purkinje Fibers, which go up the sides of the ventricles.
The name we give this electrical activity when it’s shown on a cardiac monitor is the PQRS complex, which is basically showing us one full heart beat. If you were to feel someone’s pulse and look at the monitor at the same time, you’d feel a pulsation very close to the time of each complex appearing on the screen.
So, if on TV shows you’ve heard the term, “They’re flatlining!” that means the heart has stopped beating and therefore stopped creating this important line on the heart monitor, and are essentially dying/dead unless something is done.
We have given the waves specific names. They are:
- The P wave
- The QRS complex, which consists of a Q wave, R wave, and S wave
- The T wave
By evaluating how these look on the screen or on paper, we can learn a lot about how the heart is functioning.

As I previously mentioned, we have the PR interval, QRS complex, QT interval, and the ST segment. When reading an ECG you need to interpret each wave, measure distance using the using calipers (pictured below), or you can even make small marks on a scrap of paper and then measuring using the actual graph paper, as well as determine its regularity and rate.
5-Lead ECG Interpretation
Now that we know what information this medical device is providing is, it’s time to make sense of it (interpretation).
At first, it’ll take you a bit of time to get into the habit of interpreting these. Think of it like a golf swing or assessment: Do it the same way every time. I’d like to walk you through my 5-lead golf swing!
Step 1 – Ensure the picture is clear (no artifact)
Getting a good telemetry strip is like taking a good photo. If someone is moving around quickly, the image is blurry. It’s the same with the your telemetry strip. If the patient was moving a bunch when you or the monitor tech clicked “Print,” then you’ll get a lot of artifact. Artifact shows up as a bunch of scribbly lines that don’t really make sense. You can’t interpret a strip with artifact, so you’ll need to get a new one.
Step 2 – See if the heart rate is regular
I do this by finding each R wave (the very peak of the QRS complex) and see if the space in between each R wave is the same. You can use a set of calipers or even a small piece of paper. Mark the space between two R waves and see if the others compare. If they have the same distance in between them, the rhythm is considered regular. Some people call this, “making sure the R’s march out”.
Step 3 – Check out your P wave situation
The first P wave related question is to check if there is one! Ideally, there is a P wave before every single QRS complex and that distance between the two is the same for all of the complexes on the strip. The P waves should all look the same and be regular
Step 3.5 – Measure your PR interval
As we continue to assess the P wave situation, we want to see how far it is between the P wave and the R wave (called the PR interval, or PRI). It is the distance from the start of the P wave to the beginning of the QRS complex. It should be between 0.12-0.2 seconds. Notice if each complex on your strip has the same PR interval, or if it’s different.
The PR interval is the conduction up through the AV node.

Step 4 – Check out your QRS situation
Things to notice about your QRS complex:
- Are they the same height? Do they all look the same, or does it vary?
- Is the R to R distance consistent?
The QRS complex represents the spread of the electrical impulse through the ventricles. So, we want to see consistency in shape, size, and timing.
Step 4.5 – Measure the QRS complex
Let’s look specifically at the width of the QRS complex on the line. Because its so small, tiny differences may not be obvious, so we really need to measure to check. A normal QRS complex is 0.08-0.1, and is measured from the beginning of the Q wave to the end of the S wave.
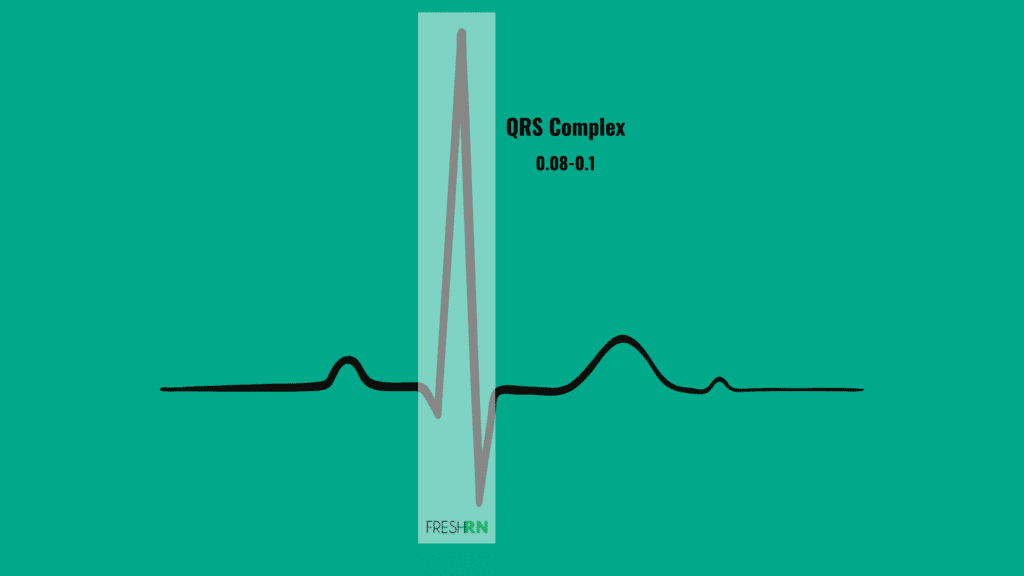
If all of the QRS complex’s on the strip look the same, are the same size, and have an equal distance between each R wave, that’s great!
Step 5 – Check in on the T and S waves
During your normal daily checks on a 5-lead monitor, you’re not going to routinely measure your T or S wave. You’ll check to see if a T wave is present, and if it’s upside or not (referred to as an “inverted T-wave”.
Note if there is elevation between the S and T. You may have head of “ST elevation” before, and that’s pretty serious and indicative of a myocardial infarction. Below is an example.

So, what’s the verdict?
The hope is that the patient has a “normal” reading. This would be referred to as “normal sinus rhythm”. That means the SA (sinoatrial node) node is sending electrical signals and they’re getting to all of the appropriate locations and the heart beats accordingly. (Normal sinus rhythm).
My abbreviated checklist for normal sinus rhythm:
- P wave before every QRS
- P waves are the same size/look the same
- PR interval is between 0.12-0.20
- R to R distances are all equal
- QRS following all P waves
- QRS complex is 0.08-0.1
- T wave is present and right side up
- No ST elevation present
If all of that is accurate and the heart rate is between 60-100 beats per minute, then we can officially call it normal sinus rhythm!
Common Abnormal Rhythms You Will Probably See
Many patients will have normal sinus rhythm, but many will not. There are a plethora of different heart rhythms you may see, but let’s go through some very common ones.
(Pst – I dive a little deeper into this in this mini course, and dive all the way in with this full ECG review.)
Sinus Tachycardia (ST)
This rhythm has all the waves and is the proper measurements but is occurring consistently at a rate faster than 100 BPM. Sometimes, if the rate is really fast, it is difficult to read all the waves. There is an option on 12-lead ECG machines and some cardiac monitors that will allow you to slow the rhythm down and stretch it out. This allows you to see all the waves if they are present.
The signals are still being sent from the SA node, but the SA node is depolarizing faster than normal. The most important thing to understand about ST is that the heart’s cardiac output is decreased and so is coronary artery perfusion – yikes!
Often the patient is dehydrated and the first line of treatment will be administering IV fluids. If the patient does not respond to IV fluids then further investigation is needed. For example, is the patient febrile? Getting the temperature-controlled will also bring the heart rate back to a normal rate. The treatment for sinus tachycardia is to eliminate the factor that is causing the heart to beat so fast.
Below is a list of things that can cause ST in patients:
- Hypovolemia (dehydration)
- Fever
- Caffeine
- Stress
- Pain
- Hypotension
- Hyperthyroidism
Before sounding the alarm to the physician, remember that fluctuations in heart rate are normal with pain and activity. While anything over 100 BPM is considered tachycardia, patients who are walking after surgery for the first time or experiencing severe pain after having a lobe of their lung removed could have a heart rate in the 130’s or even up to 150. However, if this does not calm down with rest or pain medication, it likely will require intervention.
Regardless, if someone has sinus tachycardia, it’s important to know if they have any symptoms like dizziness, light headedness, pounding chest, feeling their heart racing, shortness of breath, and so forth.
🎓 Ready to go beyond the basics?
If this feels like a lot (and trust me, it is!), you’ll love ECG Rhythm Master: my self-paced course that walks you through ECG interpretation step-by-step with visuals, practice rhythms, and 7.0 contact hours. 👇 Learn more and join the 1300+ students inside! 👇
Sinus Bradycardia (SB)
This rhythm also has all the waves but is slower than 60 BPM. This number needs to carefully be considered as people have resting heart rates at 50 BPM that are completely normal, especially if they are athletes. (The heart is a muscle, so if someone regularly works out their muscle with cardio exercise, it will beat more efficiently.)
The signals from the SA node are depolarizing at a much slower rate than normal in this rhythm. It is generally caused by stimulation of the parasympathetic nervous system (vagal). If the patient is experiencing sinus bradycardia, the time their heart spends in diastole in greatly increased and the cardiac output is decreased.
The most important thing to assess for a patient in sinus bradycardia is whether they are symptomatic or not.
Symptoms include:
- Dizziness
- Weakness or fatigue
- Altered mental status
- Shortness of breath
- Hypotension
If the patient is symptomatic, this is an urgent situation. You may need to give the patient some oxygen and prepare for potential transcutaneous pacing by pulling the crash cart over and hooking the patient up to the electrode pads.
The first line treatment depends on if the patient has a heart transplant or not. If they do not have a heart transplant and it is their original heart, prepare for the doctor to order 0.5 mg of Atropine. Atropine can be repeated every 3-5 minutes and has a maximum dose of 3 mg (6 doses of 0.5 mg). If the patient has had a heart transplant, the first-line treatment is isoproterenol (Isuprel).
If the first line doesn’t work, the second line is transcutaneous pacing. If transcutaneous pacing is not available, the doctor might order an IV drip of epinephrine or dopamine.
If the patient doesn’t have any symptoms (asymptomatic), then the physician may just want to monitor and not intervene. Generally speaking, asymptomatic sinus bradycardia is not concerning.
Think about it: if they’re not having any symptoms (dizziness, hypotension, weakness, AMS, etc), that means they probably have adequate cardiac output and therefore don’t require any intervention.
Tip – if your patient has a resting heart rate that’s pretty low and you’ve notified the physician, make sure you ask them when they’d want to be notified. This is especially helpful on the nursing floor when you have patients whose heart rates will dip down into the ’30s when sleeping. If the physician isn’t worried about it, just get an order for when they’d like to be notified again. Chances are, it’ll be if they become symptomatic. This will save you and your next shift quite a few unnecessary pages.
Premature Ventricular Contractions (PVCs)
Premature ventricular contractions (PVCs) occur when the ventricles receive an impulse prematurely, therefore they contract before they are supposed to, thus interrupting the cardiac electrical cycle. They can be harmless and common, however, they can also spark electrical chaos within the heart that can be harmful.
The more frequently PVCs occur, the more concerning they become. If the patient has two in a row, this is called a couplet.
A PVC may also occur every second beat (called bigeminy), every third (called trigeminy) or every fourth beat (called quadrigeminy).
If a patient has three or more PVCs in a row it is considered Ventricular Tachycardia and this is life-threatening.
With PVCs, the QRS complex is wider than 0.1 seconds and the R to R measurement is not regular from the other R to R measurements (the PVC comes earlier than it is supposed to).
Premature ventricular contractions will need to be monitored for frequency and treatment isn’t generally needed until the PVC occurs too frequently turning into Ventricular Tachycardia.
Tip – if you’re working at the bedside and see that PVCs are increasing in frequency, that’s a notify the provider kind of situation. Check their electrolytes (like potassium and magnesium) to see if they’re out of range, as that will likely be one of the first questions they ask you. Also know if they take any meds at home
Atrial Fibrillation (A-fib) and Afib with Rapid Ventricular Response (RVR)
Atrial Fibrillation occurs because the signals in the atria are chaotic, causing the atria to quiver. A clear contraction of the atria does not occur, thus the P wave will be absent. In place of the P wave, there will be erratic scribbles. The ventricles receive confusing signals for when to contract so they contract irregularly as well.
This is why with afib, you will have an irregular heart rhythm and no clear P wave.
The biggest problem with atrial fibrillation is the blood pooling in the atria causing blood clots to form and then sent into the bloodstream throughout the body, which is why the goal is always to get a patient back to normal sinus if possible. The treatment pathways for this depend on quite a few things, which we won’t get into the weeds of here.
If the heart rate is controlled (less than 100 BPM or so) and the patient is has no symptoms, patients can live with afib, taking an anticoagulant to prevent blood clots from forming. (However, again, the priority will be to attempt to convert them back to normal. If they cannot, it’s not a death sentence by any means. Many people live with controlled afib for many years.) However, if the patient is symptomatic and/or the rate is uncontrolled (consistently over 100 BPM) they will need treatment.
An uncontrolled afib rate is anything above 100 BPM and is called afib with RVR (atrial fibrillation with rapid ventricular response). These patients will likely be symptomatic and may feel like their heart is racing like they might pass out, dizziness and/or shortness of breath. Afib w/RVR is also called in the clinical setting SVT w/ RVR or just SVT. Dealing with this clinically can be tricky, because it’s not a true emergency like asystole (the heart stopping entire) but it’s also not benign either. It’s more of an urgent situation bedside nurses are expected to confidently handle. I had a tough time getting to that point many years ago, so I created a little (free!) email course to walk you through the steps. You can sign-up for it below. ⬇️
Atrial Flutter (A-flutter)
This arrhythmia is easily recognized because of the sawtooth pattern that appears on the 5-Lead and 12-Lead ECG. In aflutter, the conduction path from the sinoatrial (SA) node to the atrioventricular node (AV node) is spiral in nature and no longer the smooth direct pathway. The impulse still reaches the AV node causing the ventricles to contract and the QRS complex to appear at a regular interval.
Aflutter and Afib are very similar. Aflutter can turn into afib. The signs and symptoms, as well as the treatment for aflutter, are the same as the treatment for afib.
Want to level up your nursing career? Use our partner’s free tool to find accredited programs near you ⬇️
5-lead ECG Placement
Ok, let’s say you are on your cardiac unit and you’re admitting a patient who now needs continuous cardiac monitoring. Other names for this include placing a patient “on the monitor,” “monitored,” or on telemetry. Knowing 5 lead ECG placement is critical to a fast and efficient admission.
How do you place them on the monitor exactly?
You’ll have to obtain a telemetry box, leads, and pads. You’ll first place the adhesive pads on their skin in the below locations. Then, you’ll attach the appropriate leads. Next, you most likely need to call whichever unit in your hospital continuously monitors these (if that’s how your organization does things!) to confirm the patient, their information, and that they can see the tracing on their end of things.
If your patient has a pacemaker or skin issues, you may need to place your pads in alternative locations that we’re not going to dive into here.
Below is the anatomical location of each lead:
- White is on the right side, just below the clavicle (midway)
- Black is on the left side just below the clavicle
- Brown is in the 4th intercoastal space, just to the right of the sternum
- Green is on the right on the lower edge of the rib cage
- Red is on the left of the lower edge of the rib cage
A little rhyme I use to remember 5-Lead ECG placement is:
- Smoke over fire – (black over red)
- Clouds over grass – (white over green)
- Chocolate on the stomach- (but you must remember that it’s not on the actual stomach but on the right sternal boarder of 4th intercoastal space)
That may help you remember this in the moment as you’re attaching leads to a patient’s chest.
There you have it, 5 lead ECG placement simplified.
12-Lead ECG vs. 5-Lead ECG
Most cardiac patients are on a telemetry monitor. This means they’ve got 3 to 5 leads (wires that are connected to things that connect to adhesive pads) attached to their chest, and you can see their rhythm at all times at the nurse’s station and/or the bedside monitor. Most of the time it will be 5 leads rather than 3.
The difference between them comes down to the amount of detail and continuous monitoring.
A 12-lead ECG is not something that stays on the patient. Leads are attached to the patient, they get a detailed snapshot of the electrical rhythm of the patient, and then they are removed.
A 5-lead is a less detailed picture, but it’s a continuous live feed of the electrical activity of their heart.
A good comparison would be the 5-lead is like a TikTok Live, while a 12-lead would be like a high def regular TikTok video. The live feed gives you real-time updates, but the quality isn’t nearly as good or detailed as a professionally produced HD video, even if it’s much shorter.
Another way to think about it is each lead like a camera, taking a snapshot of the heart’s electrical activity. Twelve cameras provide substantially more information than five.
Make sense?
Bedside nurses are responsible for monitoring these rhythms, watching for changes and notifying the physician regarding changes and concerns. A 5-lead provides a lot of information, but if something concerning is noted, a 12-lead ECG is ordered to provide even more.
You may ask yourself: Why don’t we just continuously monitor with 12 leads all the time?
That is a very good question! Well, that’s a lot of leads to constantly have on someone to get tangled up in, it’s incredibly expensive, and not medically necessary. The 5-lead provides plenty of information for routine monitoring.
So, if your patient is having new chest pain, a new cardiac rhythm, was started on a specific cardiac medication, had a procedure, is decompensating, or a plethora of other possibilities, the physician may order a 12-lead ECG. Depending on where you work, the bedside nurse may complete the 12-lead, or an ECG tech (a person whose job it is to obtain ECGs on people all day, traveling from room to room) may come to complete the procedure. It’s pretty quick, and it honestly takes longer to attach all 12 leads than to get the reading. ECG techs are pretty awesome at these because they do them all day and can get them done very quickly.
Unit-specific nursing responsibilities
Regardless of where the patient is, many hospitals require patients on a heart monitor to have a 5-lead strip documented every shift and with any rhythm changes or significant patient events (like a code). But, how this is done depends on the unit.
If you’re working on a cardiac floor, typically a monitor technician in a different location will print and interpret your strips for you, and you simply verify them in your documentation and make corrections as needed. A monitor tech is someone whose job is to watch many 5-lead telemetry strips at once, document, and notify the nurse as changes occur. This is necessary because nurses on the floor are caring for many more patients and their patients are not on a bedside monitor for them to be able to visualize immediately. Typically a monitor is at the nurse’s station, but not in each patient’s room.
If you’re working in a step-down or intensive care environment, you most likely print and interpret your own, then document appropriately, without the back-up of a monitor technician. Cardiac monitors are typically in the room and at the nurse’s station.
The ED environment is a bit different. Patients are coming in and need to get diagnosed quickly. Therefore, as an ED nurse, you’ll be dealing with more 12-lead ECGs on a regular basis. Not all patients will necessarily be hooked up to a bedside monitor, but if they came in with cardiac concerns, they will be.
12-Lead ECG Interpretation – is it necessary for new nurses?
Ok, now that you’ve got the leads attached and have hit “record” an obtained the ECG – what do you do with it?
Twelve-lead ECGs typically come with an interpretation at the top that the machine automatically generates. This is not always correct and you cannot rely on it to accurately interpret the rhythm.
If you want to get into the deep details of reading 12-leads, there are many courses available for this. Your hospital may offer specific ones (I’d check into that first before buying anything).

Speaking as a bedside nurse, the priority is to learn how to interpret your 5-lead telemetry strips as well as knowing when something concerning is going on with a 12-lead. However, this can get INCREDIBLY detailed. When you are at this stage in your career of just learning how to keep your head above water in cardiac patient care, save learning the origins of myocardial infarctions and changes in specific leads and whatnot for when you are ready. Focus on recognizing rhythm changes, assessment skills, patient care, meds, and chatting with physicians about what to do first. Then dive into the more complicated information.
Yes, it is important to notice things like ST-elevation on an ECG – especially in the emergency department. But there’s a difference between identifying that major issue and being able to closely evaluate a very complex EKG. Expecting a newbie nurse to not only do that, but know appropriate interventions and quickly facilitate them is unrealistic.
Please don’t feel like an incompetent nurse if you can’t quickly interpret a 12-lead someone shoves in your face two weeks into orientation. The first time I really got my brain around getting deeper into 12-leads was when I was studying for my national critical care certification (CCRN) in 2015, five years into my career.
You may run into nurses who think every nurse should know how to do this at the beginning. However, learning the intricacies of a 12-lead before you’re confident in your basic cardiac patient care is like learning how to dunk before learning how to dribble.
Phew, that was a lot! More resources for cardiac confidence 👇
Thanks for getting all the way through that MASSIVE blog post. I hope you found it helpful. Cardiac nursing is especially challenging, which is why I have so many resources on it. Check them out below!
- Afib with RVR: Nursing Responsibilities – FREE email course
- Telemetry Basics Brush-Up – mini course
- ECG Rhythm Master – self-paced online course that dives deep into ECG (7.0 contact hours)
- Cardiac Confidence: A Crash Course for New Cardiac Nurses – a comprehensive cardiac crash course (11.0 contact hours)
Starting out in neuro can feel overwhelming. Our new neuro nurse review course helps beginners master assessments, spot subtle neuro changes, and build confidence fast.
Continue Reading New Neuro Nurse Review Course for Beginners: From Brain Bleeds to Bedside Care
Looking for an ortho nursing refresher course? Learn what to look for in a solid review program and see how Ortho STRONG can help you feel confident fast in orthopedics.
Continue Reading Ortho Nursing Refresher Course: A Fast-Track Review for Nurses
Feeling overwhelmed as a new grad in the ICU? A new grad ICU nurse refresher course can help you master critical care essentials, build confidence, and hit the ground running.
Continue Reading New Grad ICU Nurse Refresher Course: Master the Essentials Fast
Wondering if your preceptor is just tough, or actually toxic? Here’s how to spot the red flags of bullying, protect your mental space, and navigate this tricky dynamic like a pro nurse (without losing your mind).
Continue Reading Is Your Preceptor a Bully? Here’s How to Tell and What to Do
Let’s talk about what a med surg refresher course for new grad nurses should cover (and why med surg Mindset can help you feel confident fast)!
Continue Reading Med Surg Refresher Course for New Grad Nurses: What to Look For + My Top Pick
Curious about the connection between informatics and nursing? Learn what informatics nurses do, where they work, and how to become one in this career breakdown (plus how AI is shaping the future of nursing).
Tired of Googling rhythms and hoping no one notices? 👀

You know your meds, how to insert a foley, and the side effects of a beta-blocker—but when it comes to rhythm interpretation, it’s like a foreign language. Don’t worry—you’re not behind. You just need the right teacher.
Taught by Will Kelly, a nurse practitioner with real-world experience in tele, ER, and inpatient care, this course walks you through everything you actually need to know. No overwhelm. No assuming you’re already a pro.
Just simple, straightforward training that finally makes cardiac rhythms click—so you can feel confident at the bedside.
Start Lesson #1 Now






These are good tips to refresh my knowledge since I don’t regularly work with EKG interpretations.
impressive research and thanks for sharing!
Great information on some difficult material – will really help both new registered nurses as well as those one or two years in to refresh their memory!
So glad! 🙂
Thanks🙏